While current treatments for fistulas in Crohn’s disease patients have often led to unsatisfactory results, new stem cell-based therapies, specifically mesenchymal stem cells (MSCs), have shown great potential, a review analysis has found.
The study, “Mesenchymal Stem Cells to Treat Crohn’s Disease with Fistula,” was published in the journal Human Gene Therapy.
Crohn’s disease patients often develop fistulas, and anorectal fistulas are the most common type. Treatment for fistulas includes surgery — such as fistulotomy, ligation therapy, and anal fistulectomy — although patients often relapse and new fistulas appear. Given this, Crohn’s disease patients need alternative therapy options.
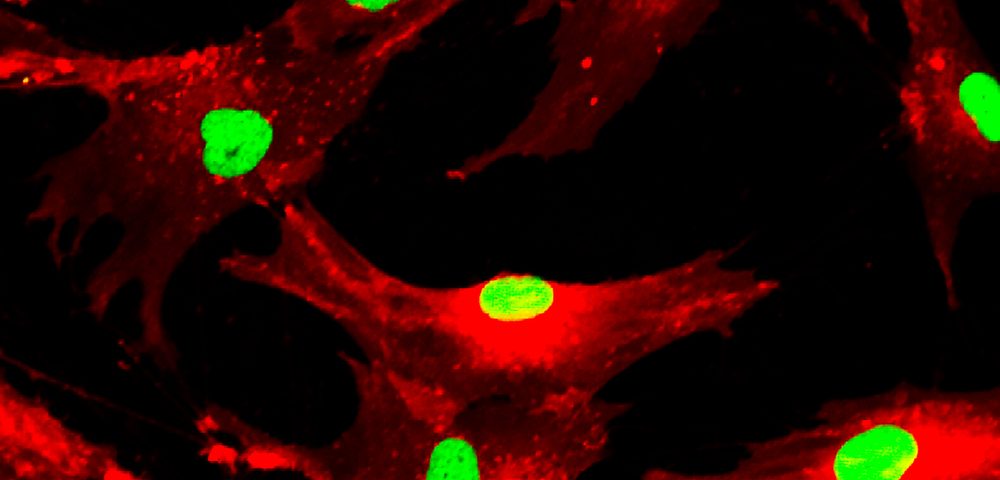
“Stem-cell therapies have recently been proposed as a method to address the challenges and prospective medical needs of Crohn’s disease patients in general and those with fistulas,” the study’s authors wrote. This method includes infusions of mesenchymal stem cells (MSCs) or hematopoietic stem cells (HSCs).
The authors reviewed several studies that suggest that MSCs could improve Crohn’s disease and Crohn’s disease-related fistulas. They point to several unique advantages of using MSC-based therapy for Crohn’s disease, including that they are easily obtained and leave no major mark at the harvesting site, while carrying a lower probability of virus infection.
Moreover, using patients’ own (autologous) MSCs means that there is less of a risk of prompting an immune reaction, and it decreases the risk for graft versus host disease (GvHD), the authors said. GvHD is a possible complication when transplanted tissue from a genetically different person is rejected by the body.
Although few studies have investigated the mechanisms associated with the benefits of MSCs for Crohn’s disease patients, some suggest that MSCs carry immunomodulatory effects when subjected to inflammatory mediators. Also, MSCs were shown to inhibit Th17 cell differentiation, or cells involved in intestinal inflammation. These cells have been shown to exert anti-inflammatory effects.
Overall, “MSC therapy has unique advantages and significant potential clinical applications as a novel therapeutic option for Crohn’s fistula. MSC-based therapies show durable efficacy with low recurrence, even in cases for which healing was not achieved with biologics or for which conventional surgical procedures cannot be performed,” the study concluded.
“Crohn’s disease continues to be a major burden on human health despite newer immunomodulatory therapies, and Crohn’s-related fistulas are a particularly intractable problem for many patients,” Terence R. Flotte, MD, Celia and Isaac Haidak Professor of Medical Education and dean of the University of Massachusetts Medical School in Worcester, MA, and editor-in-chief of the journal, said in a news release. “This paper demonstrates promising results with mesenchymal stem cells as a novel regenerative medicine approach to this complication. The work could ultimately result in major benefits to many individuals suffering with this disease.”