Nerve cells in the gut work with the immune system to fight infections, suggesting potential therapeutic avenues for inflammatory bowel disease (IBD), say researchers at New York’s Weill Cornell Medicine.
Their study, “The neuropeptide neuromedin U stimulates innate lymphoid cells and type 2 inflammation,” appeared in the journal Nature. It shows that both the immune system and the nervous system developed in parallel to respond to infections.
“The immune system and neuronal system don’t act independently,” David Artis, the study’s senior author and director of the Jill Roberts Institute for Research in Inflammatory Bowel Disease, said in a press release.
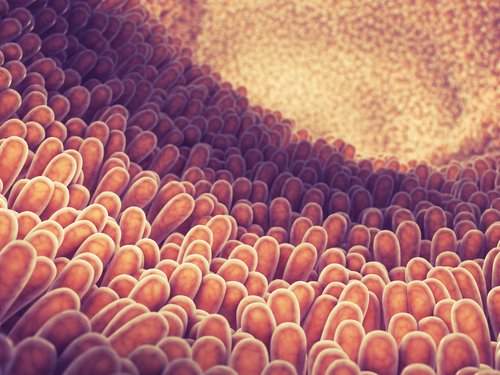
“These guys are dancing like a tango,” added Christopher S. N. Klose, the study’s lead author. The inner wall of the gut hosts a large population of immune cells, which protect against parasites and other infections while maintaining local equilibrium.
The study showed that a subtype of immune cells in the gut – group 2 innate lymphoid cells (ILC2s), which produce pro-inflammatory molecules called cytokines — are intertwined with cholinergic neurons which produce the neurotransmitter acetylcholine. The results uncovered a mechanism through which the nervous system and the immune system communicate. Specifically, the cholinergic neurons contain and release neuromedin U (NMU), a small protein that binds to receptors located in ILC2 cells.
In both in vitro and in vivo work, the scientists observed that NMU activated and caused ILC2 cells to multiply. Importantly, giving NMU to mice infected with a gut parasite induced a powerful immune response that expelled the parasite.
Furthermore, genetically deleting the NMU receptor resulted in rapid accumulation of the parasite in the gut. Adding healthy ILC2 cells (with the NMU receptor) to these mice restored their ability to expel the parasite and further proved that NMU derived from nerve cells triggers a protective mechanism by activating ILC2 cells.
“Where we are most excited is thinking about multiple chronic inflammatory diseases that might be related to this neuronal-immune axis and where we might be able to intervene,” said Artis. Although it’s still too soon to know whether treatments targeting NMU could be developed, he suggested that researching these mechanisms might generate new therapies for inflammatory diseases including IBD, asthma and food allergies.