In a new study entitled “Single-pulse and unidirectional electrical activation of the cervical vagus nerve reduces tumor necrosis factor in endotoxemia,” scientists discovered that a low-level electrical stimulation of body’s vagus nerve reduces systemic inflammation. These findings unveil the therapeutical value of bioelectronic medicine in inflammatory diseases such as Crohn’s disease. The study was published in the Bioelectronic Medicine journal.
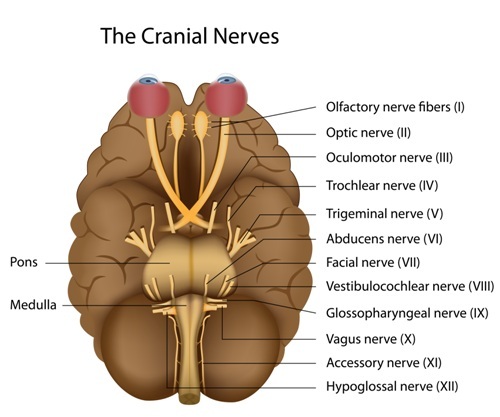
The body’s inflammatory reflex is controlled by the vagus nerve, however, scientists did not know which vagus nerve fibers controlled the inflammatory reflex. The vagus nerve, also known as cranial nerve X, is the longest of the cranial nerves and is part of the involuntary nervous system, thereby controlling unconscious body procedures such as keeping the heart rate constant and controlling food digestion. In this new research, a team of scientists at The Feinstein Institute for Medical Research, together with researchers of the North Shore-LIJ Health System (one of the largest integrated health systems in the United States), and SetPoint Medical Inc. (a biomedical technology company developing implantable neuromodulation devices to treat debilitating inflammatory diseases) investigated the role of vagus nerve fiber stimulation in reducing inflammation.
They performed studies in both mice and rats by stimulating the cervical vagus nerve with electrical impulses. The scientists hoped that this low-level electrical stimulation in the vagus nerve resulted in a reduction in the body’s inflammation.
The team first discovered which vagus nerve fibers control are activated upon vagus nerve stimulation. They then performed additional studies and found that a single electric stimulation impulse of low-intensity and during a short-interval reduced the production of inflammation-inducing cytokines, such as tumor necrosis factor alpha (TNFα), a key cytokine involved in systemic inflammation.
Dr. Kevin J. Tracey, president and CEO of The Feinstein Institute for Medical Research commented, “Identifying the exact role of the different nerve bundles in the inflammatory reflex bolsters our understanding of the relationship between the central nervous system and the vagus nerve. Furthermore, we now know that stimulating the vagus nerve for as little as half a millisecond is enough to inhibit tumor necrosis factor (TNF) production.”
Yaakov Levine, PhD, senior research scientist, SetPoint Medical Inc. added, “Seeing successful results with low-level electrical current is a significant finding. This indicates the potential for limited side effects, as well as promise for device miniaturization, both of which will be important to bringing vagus nerve stimulation into the mainstream.”
The findings establish the potential of using bioelectronic medicine, where molecular medicine is combined with bioengineering, as a new therapeutic for inflammatory diseases.