Researchers at UT Southwestern Medical Center found that a cellular mechanism called autophagy is an important participant in the protection of mouse intestines from inflammation triggered by invading bacteria.
These findings were featured in a study titled “Paneth cells secrete lysozyme via secretory autophagy during bacterial infection of the intestine,” published in the journal Science.
“This is the first example of this alternative pathway [autophagy] being used in immune defense in any kind of animal,” Dr. Lora Hooper, chair of immunology at UT Southwestern, an investigator at the Howard Hughes Medical Institute, and senior author of the study, said in a news release.
Autophagy is a process commonly involved in the destruction of unwanted or potentially harmful components in cells.
Previous studies showed that mutations affecting a gene involved in the autophagic pathway known as ATG16L1 was a common feature in patients with Crohn’s disease. However, until now it was not fully understood how autophagy could contribute to the development of inflammatory bowel disease.
The research team, led by Dr. Lora Hooper, investigated what happened in mice genetically engineered to carry ATG16L1 mutations similar to those described in Crohn’s patients when exposed to Salmonella bacteria carried by food.
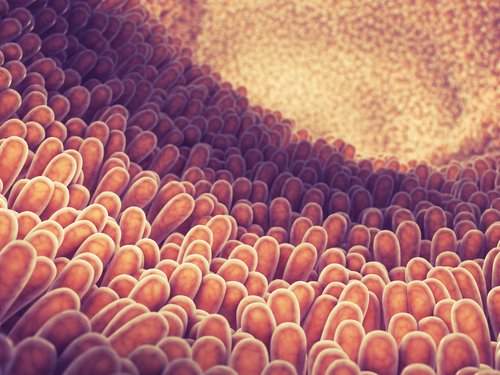
They found that the mice bearing the mutations were unable to defend the intestines from the harmful bacteria. Indeed, the cells lining the intestines could not produce small antibacterial compounds and that work as a secondary protective barrier against bacterial invasion.
In control animals that did not have the genetic mutations, the researchers could see that this secondary line of defense was intact. The intestine’s cells could produce and release the tiny antibacterial compounds and provide that additional protective pathway to the cells that were under attack by the Salmonella bacteria. These results support the hypothesis that this defense mechanism relies on the autophagy pathway.
“When intestinal cells from normal, wild-type mice encounter Salmonella, their protein weapons travel through this detour, or backup pathway, and still make it to the battle lines on the cell surface,” Hooper said. “In mice with this Crohn’s mutation, the detour pathway is blocked and unable to kill bacteria.”
“This substitute pathway uses classical autophagy machinery to make and transport protein weapon reinforcements to the cell surface after the first line of defense fails,” Hooper added.
The mice used in the study presented intestinal features that resembled those of human patients with Crohn’s patients, which suggested that the mechanism described in this study may also happen in human disease. However, no human samples were used in the study to confirm this.
“Understanding of what is going on in Crohn’s patients and the role of mutations in this backup defense system will take much more research,” Hooper said. “We believe this study provides a better understanding of what goes wrong in the intestinal lining in Crohn’s patients. Time will tell.”