Editor’s note: This is the first in a series of columns by Mary Horsley about IBD-related procedures.
For what I have been referring to as my “Scope Series,” I would like to discuss some procedures with which Crohn’s disease and ulcerative colitis patients are all too familiar.
As mentioned in a previous article, Crohn’s Disease: Journeying Toward a Diagnosis, after IBD patients meet with their physician and gastroenterologist, or GI doctor, patients likely will go through a procedure or two. Sometimes patients will undergo these before and after their diagnosis, and knowing what to expect can help the first-timers.
Procedures, like these scopes, help not only to differentiate and diagnose bowel diseases and problems for IBD patients, but they also help to check for disease maintenance or progression, check for blockages or narrowing, and help find inflammation or possible remission.
Colonoscopies and endoscopies
Often, the first procedure ordered for a patient is a colonoscopy or upper endoscopy; sometimes they are done at the same time. I have gone through three colonoscopies and two endoscopies, as sometimes more than one is needed.
These are done under general anesthesia, or conscious sedation, in my experience with the VA (U.S. Veterans Health Administration), to help avoid any discomfort or patient embarrassment.

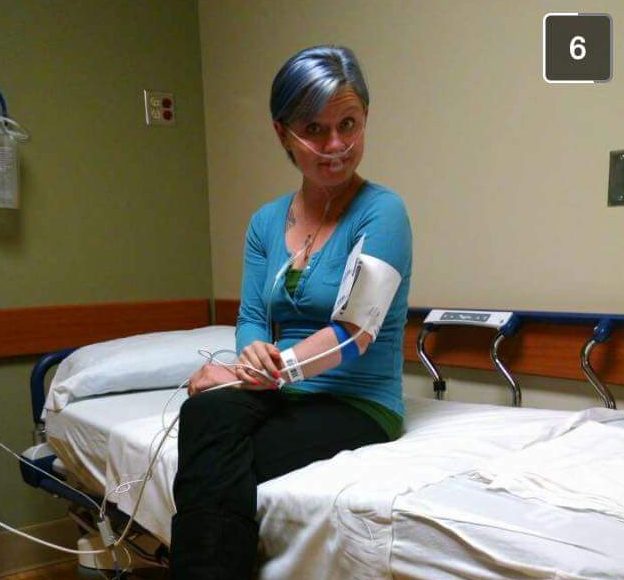
Fasting is usually required for these scopes, with a bowel prep to drink the night before. The prep is used to help clean your insides for better viewing, around 64 ounces of a thick liquid solution. In my experience, I have regretted mixing any flavoring to the mixture, but drinking with a straw helps to avoid tasting it. In the large picture above, I am preparing to take the bowel prep mixture with coloring for colonoscopy.
The colonoscopy consists of a tube being inserted into the body through the anus (up from the bottom), to look at the rectum and colon, your large intestine. You lie on your side in a hospital gown while doctors enter your rectum and view the images on a television-like screen, recording any abnormalities and taking biopsies as needed.
An upper endoscopy is where the tube is inserted via the mouth (down from the top) to look around the stomach and the beginning of your small intestine. A throat spray is used to help avoid pain and irritation,

and sometimes a brace is placed in your mouth to keep it open. It’s same general idea as a colonoscopy, just entering at a different end.
During both scopes, air is blown into your body through the tubes, allowing movement and viewing. By pumping in air the intestines are widened and more area can be seen. This air can cause discomfort and slight pain from bloating. The air also will cause you to be gassy; there is no way around it, so be warned and try to find some humor in it.
Because your stomach has so much length to it, these scopes cannot reach all portions, leaving areas of potential inflammation undiscovered. If the problem areas are not within view, other procedures are discussed.
After the scoping is complete, patients usually “wake” in a recovery room as the sedation wears off, and then you are allowed to go home. Having anesthesia, I

usually never remember the procedure or details. You’ll need a driver before you can leave the facility.
I woke up during my very first colonoscopy, and honestly, it was terrible. I woke with the tube still inside my body, feeling the doctor move around. During this specific scope, my anesthesia wore thin and I woke up in pain and distress.
The video screen in the room was showing my bowels and I remember crying, I think due to being shocked and overwhelmed, too. I could feel the air and moving around inside my stomach and it was not a pleasant feeling. Don’t let me scare you; this is not too common. I just learned the hard way that I wake early with sedation, so now I warn them beforehand.
Not only have I gone through a number of scopes, but I have some experience with other procedures as well, like pill capsule endoscopies, a double balloon endoscopy, and, an emergency surgery for a perianal abscess that led to a fistulotomy. (I’ll discuss those procedures in upcoming columns.)
Getting these scopes can help your diagnosis and the management of your disease and I can only suggest discussing them with your doctor. My experiences may be different than yours, but you never can be too prepared for what could happen with your Crohn’s disease or IBD.
Because for me, It Could Be Worse.
Note: IBD News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. The opinions expressed in this column are not those of IBD News Today, or its parent company, BioNews Services, and are intended to spark discussion about issues pertaining to inflammatory bowel disease.


