Last in a series. Read part one.
In last week’s column, my hope of getting a COVID-19 vaccine was slowly chipped away while I navigated the difficult process. Almost two weeks after our governor, Greg Abbott, announced that my group, Phase 1B, should be vaccinated, I couldn’t find the vaccine anywhere. The Texas Department of State Health Services wouldn’t release an updated list of vaccine distribution centers until Monday, so I wasn’t going to fret about it over the weekend.
Don’t call us, we’ll call you.
On Saturday morning, my fitness tracker alerted me of an incoming text. Without my glasses, all I could make out was a San Antonio phone number and something about COVID-19. I dragged myself out of bed to check my phone, assuming the message was about vaccine delays.
With my toothbrush in my mouth, I cheered as I read that my transplant hospital had enough doses for established patients. Did I want one?
I excitedly responded for an appointment scheduler to call me. I didn’t expect to hear from anyone until later in the week. Surprisingly, someone called on Sunday morning. I could have made my appointment for 8 a.m. on Friday, but despite my eagerness, I didn’t want to wake up at dawn and battle rush hour traffic on the 80-mile stretch connecting Austin and San Antonio. I settled for an appointment on Friday at 2 p.m.
Although I was ecstatic, I felt guilty for having the vaccine offered to me while others continued to run into dead ends. I shared the news of my appointment only with my immediate family members and a close friend, a nurse, who recently had been immunized at work.
V-day arrives.
Later in the week, I discovered that my gastroenterologist’s colleague had discouraged people from getting the COVID-19 vaccine within 48 hours of receiving a biologic. My Remicade (infliximab) infusion was about 30 hours before my appointment. I wasn’t too concerned and had planned to go to the vaccine clinic alone. My husband was worried I might experience side effects on the drive back, so he took the day off to accompany me.
When I entered the hospital, a screener in the lobby took my temperature, handed me a visitor tag for the vaccine clinic, and told me to have a seat. After she had a group of four patients, she instructed us to go down the hallway. A group of nurses greeted us outside the vaccination room to record our demographics, verify our contact information, and get our verbal consent for the shot. They directed us into the room one by one.
Once inside, another nurse handed me two cards and fact sheets about the Moderna vaccine. I then waited for one of the two inoculation stations to open up. When my turn came, a nurse confirmed my identity and asked if I had had any vaccines in the past 14 days. The other nurse prepped the syringe and then pressed down on my shoulder as she jammed the needle in my upper arm. The vaccine felt no different from getting my annual flu shot.
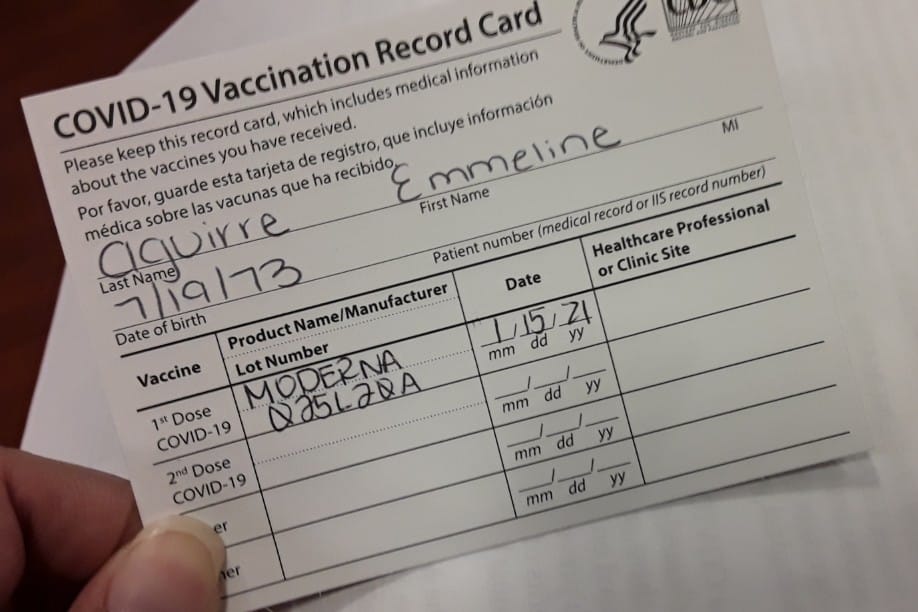
Afterward, I handed both cards to another nurse who recorded my information. She handed back my vaccine card and directed me to the observation room to make my appointment for my second dose. Before I could leave, I had to sit for 15 minutes.
Compared to the horrendous vaccine distribution system, the organization and efficiency of the vaccine clinic impressed me. The entire process took a little more than half an hour.
Two weeks down, but for others, many weeks to go.
After the first shot, I had a sore arm for a few days. I’ve heard chills, tiredness, and headache are more common with the second shot. I had a similar experience with the shingles booster. I anticipate my next dose of Moderna on Feb. 12 will be rougher.
As of Jan. 21, I’m one of only 17.6 million Americans who have received their first dose of the COVID-19 vaccine.
According to news reports, Austin Public Health has acknowledged vaccinating walk-ins “out of common courtesy.” Texas health officials are relying on “the honor system” instead of requiring proof of medical necessity. I’m infuriated that some people were able to cut in line ahead of priority groups. A friend, who is a physician’s assistant, and my husband, who has hypertension and is a 1C essential worker, can’t even get on a waiting list.
I’m hoping that with U.S. President Joe Biden’s national COVID-19 strategy to vaccinate 100 million Americans within his first 100 days in office, the next three months will look a lot different from the first six weeks of the vaccine rollout.
***
Note: IBD News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health providers with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. The opinions expressed in this column are not those of IBD News Today, or its parent company, BioNews, and are intended to spark discussion about issues pertaining to IBD.