Last week I had my annual colonoscopy. I had some mild inflammation, but my condition has remained stable since last year.
My husband told me that as soon as I woke up, I asked the nurse, “Can I go to work now?” I don’t know what job I thought I was going to considering I work from home. Thankfully, my husband took the day off. Otherwise, I might have driven to my old teaching job 40 miles away.
With my colonoscopy out of the way, I have one more test this month: my annual tuberculosis (TB) test. When I first started Remicade (infliximab), I was told I would need to be tested for TB because the medication would lower my immunity. I hadn’t fully understood the link to TB, so I decided to learn more about it.
TB is an infection caused by the bacterium Mycobacterium tuberculosis, which mainly affects the lungs. However, the infection can spread through the bloodstream and lead to complications involving the heart, liver, kidneys, and brain. It can also cause spinal pain and joint damage.
TB is a communicable disease that’s often spread between people who work or live closely together. A person also can be infected with TB without displaying symptoms or being contagious. For this reason, doctors distinguish between latent TB and active TB. With latent TB, the body’s immune system prevents it from becoming active.
The U.S. Centers for Disease Control and Prevention reported a total of 9,029 new TB cases in the U.S. in 2018, with almost 70 percent occurring in people born outside the U.S. The bacillus Calmette-Guérin (BCG) vaccine is available, but it’s generally given to infants born in countries where TB is prevalent and is not widely used in the U.S.
In addition to living in or traveling to high-risk countries, other risk factors for the disease include use of intravenous drugs and alcohol, being very young or very old, working in healthcare or in a residential care facility, or having a weakened immune system caused by other diseases or the medications used to treat them.
Some of these medications include the tumor necrosis factor (TNF) inhibitors used to treat inflammatory bowel disease, such as Remicade, Cimzia (certolizumab), Humira (adalimumab), and Simponi (golimumab). A study published in the journal Clinical Infectious Diseases found “the use of anti-TNF therapies for the treatment of inflammatory conditions … has been associated with granulomatous infections.” A granuloma is a small area of inflammation commonly seen in TB.
In this study, researchers hadn’t anticipated findings that showed that the two most widely used TNF blockers differed in their spectrum of activity and also in the “risks they pose for reactivation of latent granulomatous infections.”
A subcommittee formed by the British Thoracic Society Standards of Care Committee to examine the best approach to prevent TB in patients needing and other anti-TNF therapies recommended screening of patients for active or latent TB before beginning anti-TNF treatment.
I’ve had the relatively painless Mantoux tuberculin skin test (TST) that requires two trips to the doctor’s office. On the first visit, a small amount of tuberculin purified protein derivative, made from an inactive strain of Mycobacterium tuberculosis, was injected intradermally into my inner forearm, leaving a small bubble or bump under the surface of the skin. During the second visit, 48 to 72 hours later, the injection site is “read.” If the area is raised, hard, or swollen, the test is positive for TB.
This year, I had the option of getting the blood test. The interferon-gamma release assay (IGRA) measures the immune system’s response to M. tuberculosis. The test is completed during one clinic visit, and results are available within 24 hours. Unlike the TST, the IGRA has no risk of producing a false positive in patients who have received the BCG vaccine.
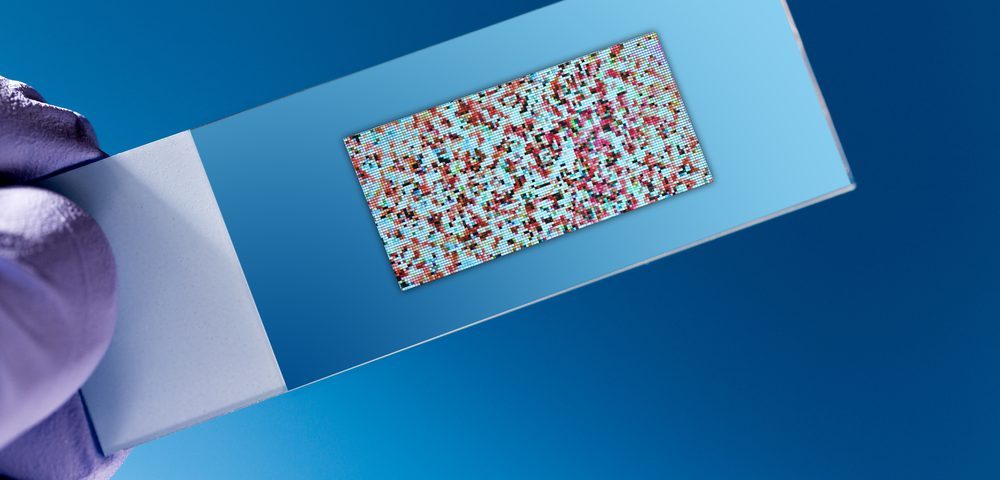
With the IGRA, white blood cells release interferon-gamma (IFN-g) when mixed with antigens — substances that produce an immune response — derived from the bacteria. Results are based on the amount of IFN-g released or the number of cells that release IFN-g, depending on which IGRA test is performed. To date, there are two FDA-approved tests, the QuantiFERON-TB Gold Plus (QFT-Plus) and the T-SPOT.TB test.
While researching the IGRA test, I discovered that the QFT-Plus test I’m having requires the blood sample to be tested within 16 hours of the draw. Knowing that my lab has to send out the sample to be processed off-site, I can’t get my blood drawn on Friday afternoon as I had planned.
Fortunately, I was able to reschedule my appointment for Tuesday afternoon, meaning by the time this column is published, I could have my results. If all goes well, I shouldn’t have to worry about any other tests other than my usual bloodwork until next year.
***
Note: IBD News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health providers with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. The opinions expressed in this column are not those of IBD News Today, or its parent company, BioNews Services, and are intended to spark discussion about issues pertaining to IBD.