New research unveils how two molecules, protein complexes called S100A8 and S100A9, are regulated in order to limit an inflammatory responses to sites where they are needed, preventing the spread of inflammation throughout the body.
The findings may help in treating inflammatory diseases, including inflammatory bowel disease (IBD), by targeting specifically S100A8/S100A9 so as not to interfere with other factors in the immune system required to fight infections.
The study, “Autoinhibitory regulation of S100A8/S100A9 alarmin activity locally restricts sterile inflammation,” was published in the Journal of Clinical Investigation.
Two much of a good thing often leads to a bad outcome, and a perfect example is what happens in autoimmune diseases, where an exacerbated response takes aim at healthy tissue.
A group of molecules expressed by tissues, called danger-associated molecular patterns (DAMPs), act as danger signals and trigger inflammation when released by activated immune cells.
Two proteins, called S100A8 and S100A9, are the most abundant DAMPs in many autoimmune diseases. But the mechanisms regulating their activity are poorly understood.
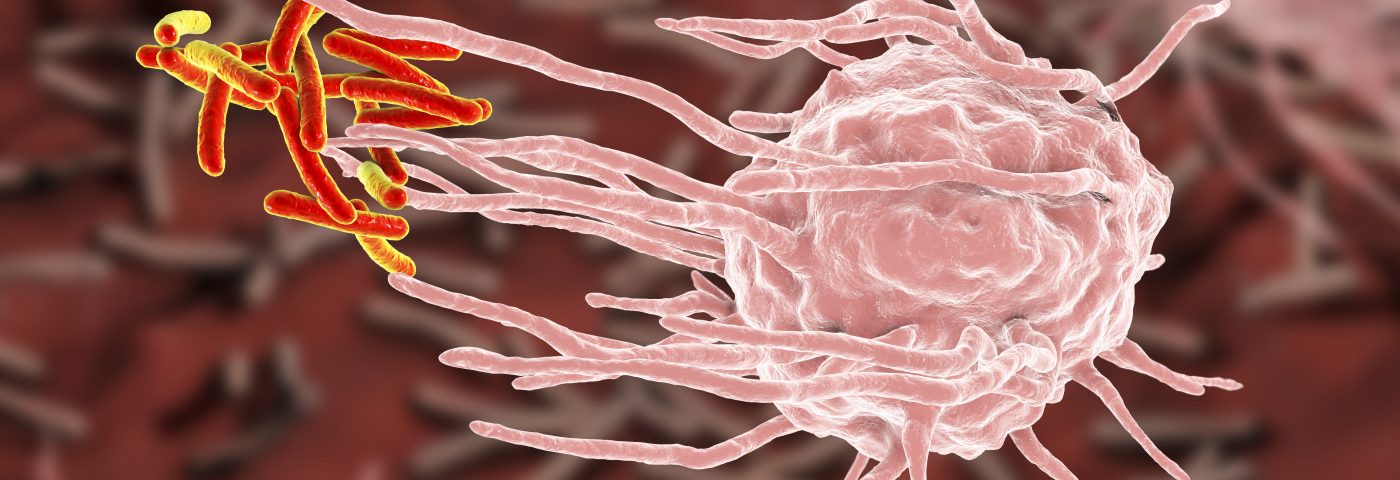
Researchers at the University of Münster, Germany, show that the proteins work together and forms complexes, called heterodimers, that are released by certain immune system cells, the so-called phagocytes, when activated.
The complexes then bind to their target receptor — Toll-like receptor 4 (TLR4) — in other cells, promoting the inflammatory process.
Importantly, the S100A8/S100A9 complex only has a short lifespan — a short period of time during which it needs to find and bind to its receptor to promote the inflammatory response. Failure to do so triggers complexes to associate with each other, culminating in their inactivation.
This mechanism is a way to control the inflammatory process and keep it restricted to a specific locations, rather than inducing generalized inflammation.
“Too many heterodimers remain active, trigger a strong immune response, and act systemically in the entire body,” Thomas Vogl, the study’s lead author, said in a press release.
These results may help researchers develop new ways to tackle the mechanisms underlying inflammatory diseases, including IBD.
Current approaches target the expression of the TLR4 receptor. But this strategy comes with a caveat, as TLR4 signaling is required to induce a proper immune response against infections.
“This is why we’re searching for antibodies which specifically only block the S100-TLR4 axis, while the receptor is untouched, respectively free on the bacterial side,” Vogl said.
“These antibodies should specifically block only the active heterodimers and weaken the immune reaction only locally, at the site of inflammation. The TLR4 receptor, which is important for immune defense, remains untouched and can trigger the suitable immune response in the case of any bacterial danger,” he added.
The team is now looking for pharmaceutical industry partners to develop antibodies and potential medicines that tackle this mechanism, so researchers can test the efficacy of this approach in preventing rampant inflammatory reactions.