Editor’s note: This is the second in a series of columns about the similarities and the differences among IBD, Crohn’s disease, colitis, IBS, and celiac disease. Read part one here.
Inflammatory bowel diseases like Crohn’s, ulcerative colitis (UC), and the other autoimmune diseases of the gastrointestinal tract can be confusing and hard to recognize.
These diseases can be so different, and yet alike, that the distinctions among them can be hard to understand. Knowing what these differences are, and which disease you or your friends suffer from, can help with understanding IBD.
While Crohn’s and UC are members of the autoimmune disease category, as is IBD, and have similarities and several differences, both are believed to be caused by factors including genetics, environment, and an immune system gone renegade. Neither has a cure.
Both involve chronic inflammation in the gastrointestinal tract and digestive system and can manifest in many symptoms, inside the body and out.
With Crohn’s, top to bottom, mouth to rectum, it all suffers. Where colitis focuses on one area, Crohn’s can skip areas, leaving healthy segments mixed with inflamed areas. Crohn’s can affect the small and large bowel, the rectum, the stomach, anywhere.
Crohn’s disease can affect any layer and any portion of the bowel, leaving ulcerations, inflammation, and many other problems. Crohn’s disease often requires more extensive scoping, as well, because of a high prevalence of small bowel inflammation.
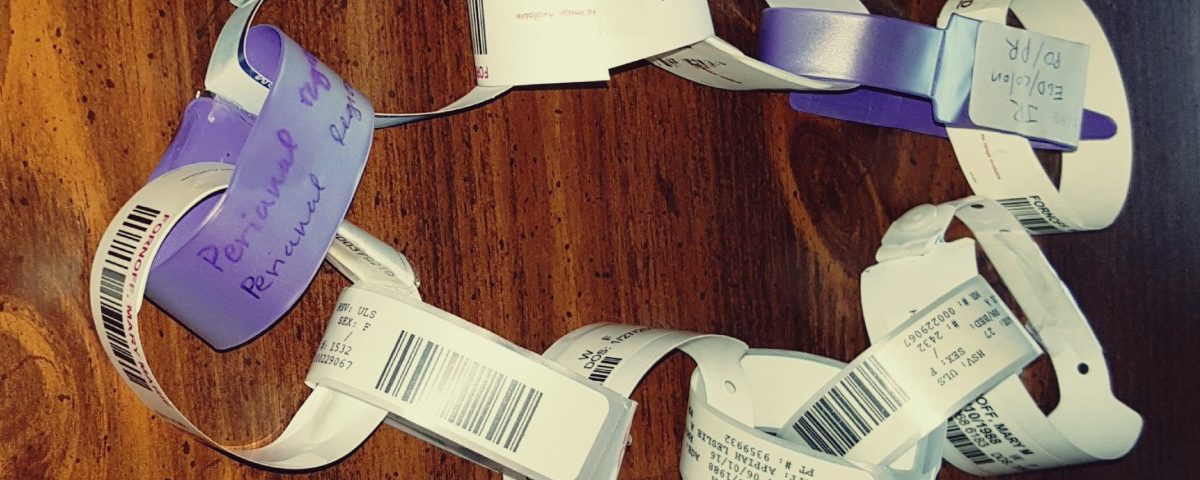
There are no specific tests to find and diagnose these diseases; often a number of blood tests and scopes are needed to aid doctors in diagnosis.

It took more than two years, five scopes, two pill capsules, two surgeries, and multiple X-rays and blood tests before my diagnosis, mainly because my Crohn’s disease is in the small bowel. I got many ideas for different diagnoses because IBD is so hard to diagnose. I am on my sixth medication and working toward my fourth year in my journey with Crohn’s. (See “Scope Series: Pill Capsule Endoscopy.”)
For me and my Crohn’s, It Could Be Worse.
***
Note: IBD News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. The opinions expressed in this column are not those of IBD News Today, or its parent company, BioNews Services, and are intended to spark discussion about issues pertaining to IBD.