New findings on inflammatory bowel disease (IBD) suggested that genetic variation is critical for determining disease severity and could provide a more personalized approach for clinical management of IBD patients. The study, “Inherited determinants of Crohn’s disease and ulcerative colitis phenotypes: a genetic association study,” was published in the journal The Lancet.
IBD affects approximately 1.6 million individuals in the U.S., including 80,000 children, according to the Crohn’s and Colitis Foundation of America. Crohn’s disease and ulcerative colitis, the two main forms of IBD, affect 1 in every 200 people in developed countries. IBD is characterized by an exacerbated mucosal immune response from the intestine tissue in genetically susceptible individuals. Several genetic studies have identified 163 susceptibility loci for IBD, including NOD2 and HLA, common to both Crohn’s and ulcerative colitis.
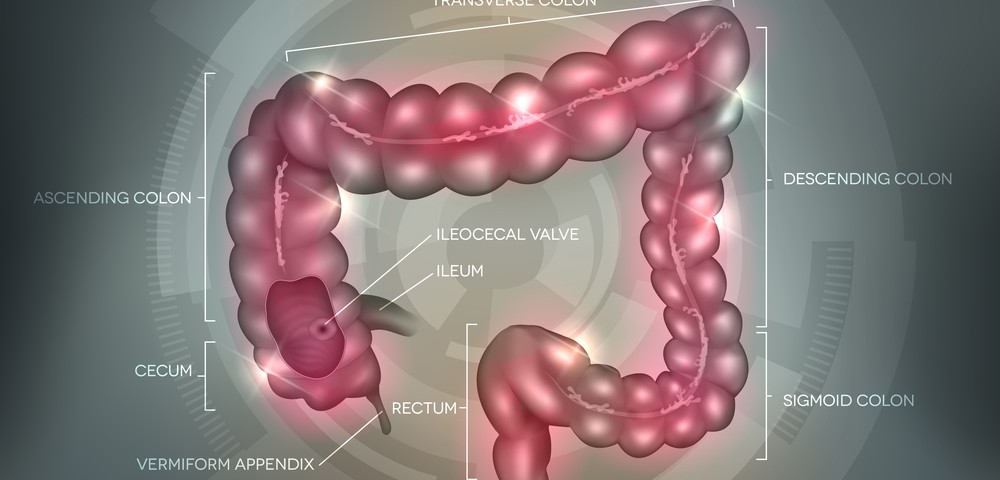
Inflammation in Crohn’s disease can occur in any region of the gastrointestinal tract, while ulcerative colitis normally occurs in the colon. The Montreal classification has been widely used to distinguish clinical subphenotypes in Crohn’s disease by disease location, behavior, and age of onset, and in ulcerative colitis by disease extent and age of onset. Surgery and drugs that restore the immune system have been considered the most efficient treatments; however, IBD is considerably heterogeneous in disease course and in individual response to therapy.
This is thought to be the largest genotype-phenotype association study to date, applying the Montreal classification to 34,819 patients with IBD from 49 centers in 16 countries in Europe, North America, and Australasia, combined with matching genotypes from more than 150,000 variants. This study aimed at better understand the genetic basis of IBD subphenotypes.
Researchers defined genetic risk scores by combining information from all known IBD associations to define the total load of genetic risk for a particular disease phenotype. They used the risk scores to test the hypothesis that colonic Crohn’s disease, ileal Crohn’s disease, and ulcerative colitis are all genetically distinct from each other, and to try to identify patients with a disagreement between clinical diagnosis and genetic risk profile.
In the study, researchers refined the known genotype-phenotype associations, such as the effect of NOD2 on disease behavior that is completely determined by its association with disease location, and discovered one new associated locus (3p21/MST1 and age at diagnosis). Moreover, for the first time, researchers investigated the genetic associations between subtypes of IBD with genetic risk scores. Their findings support IBD as a continuum of disorders, much better defined by three groups (ileal Crohn’s disease, colonic Crohn’s disease, and ulcerative colitis) than by Crohn’s disease and ulcerative colitis only (as currently defined), especially since ileal and colonic Crohn’s disease are at least as genetically distinct from each other as they are from ulcerative colitis. The team also found that disease location is an inherent aspect of a patient’s disease, partially determined by genetics, and the main driver to changes in disease behavior over time.
“This new research strongly suggests that we are dealing with a number of different diseases hidden within Crohn’s disease and ulcerative colitis, constituting a large spectrum of inflammatory bowel disease,” said Dr. Dermot McGovern, co-senior author of the study, in a press release. “We want to understand what the important, singular, genetic signature is for each individual patient because they may respond to available therapies very differently, even with the same IBD diagnosis.”
“Genetic research of this magnitude of sample size provides critical information about IBD that takes us farther down the road to providing personalized diagnosis and care to our patients with complex disorders,” added Shlomo Melmed, MD, executive vice president of Academic Affairs and dean of the medical faculty at Cedars-Sinai.
This research provides an important pathway to improved patient care for IBD and also for other autoimmune diseases, such as spondylitis and psoriasis, since genes associated with IBD have been also linked to these conditions.