In a recent study entitled “Placental inflammation is not increased in inflammatory bowel disease”, researchers investigated whether women with inflammatory bowel disease (IBD) exhibit higher rates of placental inflammation, and if this is a potential explanation for the increased risk for adverse birth outcomes usually experienced by IBD women. The study was published in the journal Annals of Gastroenterology.
Women affected by active IBD, characterized by chronic inflammation of the digestive tract, with ulcerative colitis and Crohn’s disease as its main disease types, may have increased risks for adverse birth outcomes, including preterm delivery and small for gestational age (SGA) children (of note, riskier births have also been observed in women with quiescent IBD throughout pregnancy). Thus, understanding what affects poor birth outcomes in IBD women is crucial to develop efficient and targeted therapeutics to improve births.
Here, researchers compared placental histology of women with IBD to that of women without IBD. While the majority of studies attributed the poor birth outcomes in women with IBD to disease activity, IBD medication use and nutritional deficiency studies in non-IBD women attributed birth problems to other factors, including defects in the placenta. Placental factors, however, have not been investigated in the case of IBD patients. The authors hypothesized that an increase in placenta inflammation may lead to the poor birth outcomes in IBD patients.
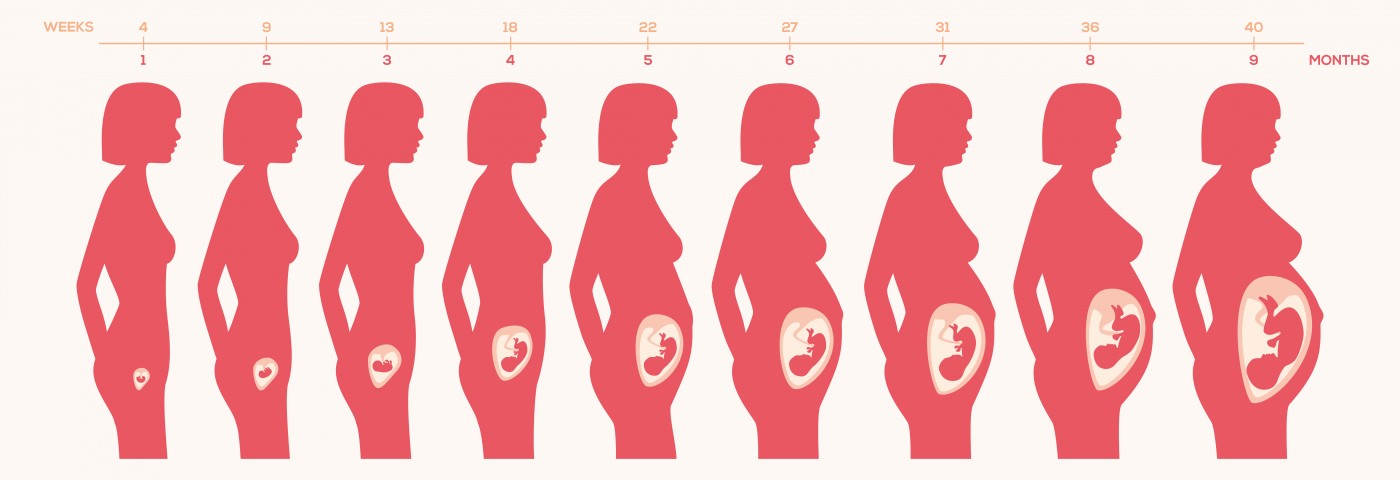
The team analyzed placenta samples from patients enrolled in the Pregnancy in Inflammatory Bowel Disease and Neonatal Outcome (PIANO) registry, specifically placental tissue of 7 ulcerative colitis, 5 Crohn’s disease, and 2 IBD patients. Additionally, they analyzed the history of birth of all IBD patients and matched it to non-IBD controls by gestational age at delivery. It was detected that among women with IBD, 29% delivered preterm infants and 21% delivered SGA infants. However, chorioamnionitis (a condition where bacteria infects the chorion and amnion, the membranes that surrounds the fetus, and the amniotic fluid) was the only placental defect authors detected in the analyzed placenta tissues. In fact, chorioamnionitis appears to occur less in IBD patients, when compared to non-IBD women.
Hence, authors highlighted that their findings suggest that placental inflammation is not the factor underlying poor birth outcomes in women with IBD, and that additional studies are required to determine the factors responsible for these poor outcomes.