A recent review entitled “Cancers Complicating Inflammatory Bowel Disease” described an association between the risk for several types of cancers in patients with inflammatory bowel disease due to chronic intestinal inflammation or immunosuppressive therapies. This review was published in the New England Journal of Medicine by Dr. Laurent Beaugerie from Hôpital Saint-Antoine in Paris and Dr. Steven H. Itzkowitz from Icahn School of Medicine at Mount Sinai.
A recent review entitled “Cancers Complicating Inflammatory Bowel Disease” described an association between the risk for several types of cancers in patients with inflammatory bowel disease due to chronic intestinal inflammation or immunosuppressive therapies. This review was published in the New England Journal of Medicine by Dr. Laurent Beaugerie from Hôpital Saint-Antoine in Paris and Dr. Steven H. Itzkowitz from Icahn School of Medicine at Mount Sinai.
“Among the chronic inflammatory diseases that often require the prolonged use of immunosuppressants, [IBD] is an intriguing model because immunosuppressants may reduce the incidence of inflammation-related cancers through their anti-inflammatory effects or promote immunosuppression-related cancers,” wrote Dr. Beaugerie and Dr. Itzkowitz, in a news release.
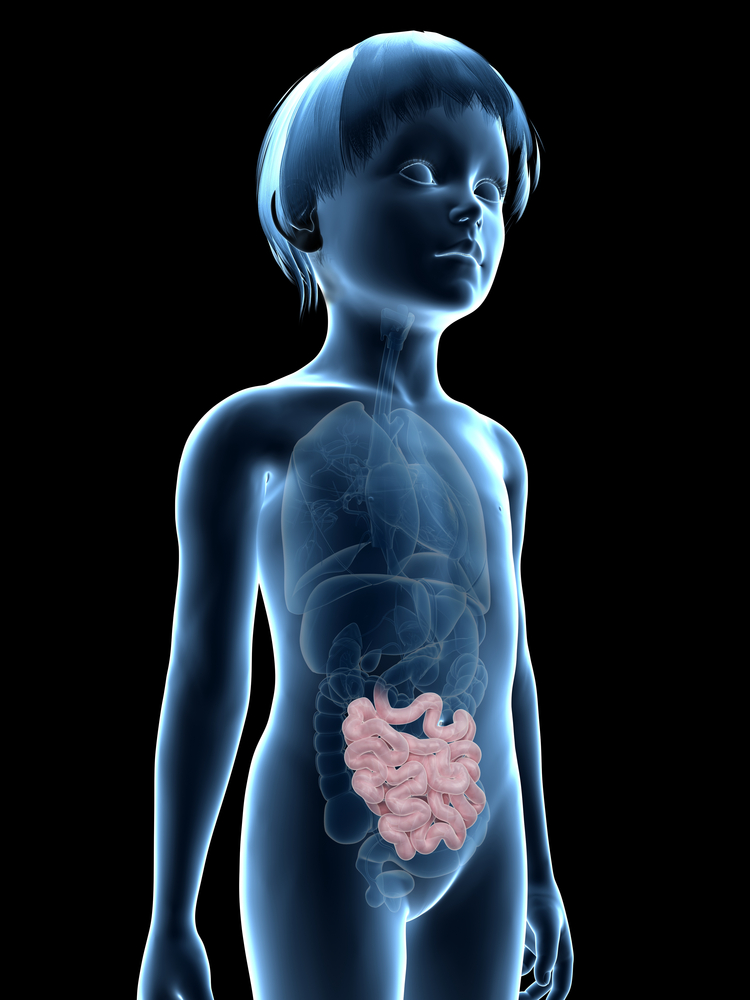
In North America and some countries in Europe, individuals with inflammatory bowel disease (IBD) and adolescents with pan colitis, a very severe form of ulcerative colitis, with the disease spreading through the large intestine from the cecum to the rectum, have 1.5 times more and 15% higher probability of developing colorectal cancer when compared with the general population, respectively.
A previous study using meta-analysis has shown that an improved control of inflammation, as well as implementation of colonoscopic surveillance and higher implementation of colectomy in some countries and possibly the use of chemopreventive 5-aminosalicylates (5-ASAs) promoted a decrease in higher probability for colorectal cancers in patients with IBD. However, there have been studies with conflicting findings concerning the potential preventive effects of 5-ASAs, thiopurines and tumor necrosis factor-alpha antagonists. Surveillance using colonoscopy is difficult in IBD patients due to the inflammatory state of the intestine.
Individuals with inflammatory bowel disease have features that increase the probability of developing colorectal cancer such as cumulative increase in colonic inflammatory lesions and active chronic inflammation by endoscopy or histology analysis.
Around 15% of colorectal cancers cases are detected in the first 7 years after the appearance of IBD, and it remains a matter of debate if the diagnosis of IBD in young individuals is a risk factor independent of IBD duration.
It has been well established that chronic inflammation is an important cause of colitis-associated cancer, while the relevance of luminal microbiota changes is presently a very “hot” research topic.
Individuals with Crohn’s disease have 20 to 30 times more probability to develop small bowel adenocarcinoma in ileal lesions after 8 years of Crohn’s diagnosis than individuals without Crohn’s. Presently, for these cases surgical removal of ileal lesions is the only preventive procedure available.