 A recent study entitled “Inflammatory Bowel Disease and Cervical Neoplasia: A Population-Based Nationwide Cohort Study” published in Clinical Gastroenterology and Hepatology reported a new link between Crohn’s disease and uterine cervix neoplastic lesions.
A recent study entitled “Inflammatory Bowel Disease and Cervical Neoplasia: A Population-Based Nationwide Cohort Study” published in Clinical Gastroenterology and Hepatology reported a new link between Crohn’s disease and uterine cervix neoplastic lesions.
The authors aimed to investigate a possible two-way association between inflammatory bowel disease (IBD), particularly its most common manifestations — Crohn’s disease and ulcerative colitis — with Cervical Neoplasia.
For this study, the team analyzed a national cohort of women arranged in three groups: Crohn’s disease (which included 8717 patients), ulcerative colitis (which included 18,691 patients) and a control group (which included 1,508,334 women from the general population).
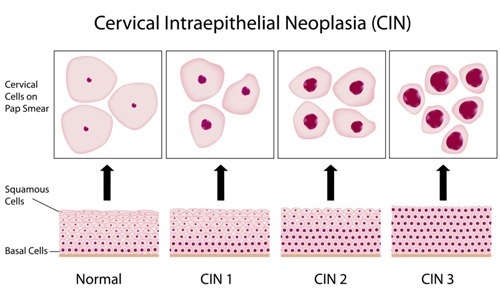
While women with Crohn’s disease and the control group received cervical cancer screening with the same frequency, in ulcerative colitis patients, the frequency was increased. During a follow-up of approximately eight years, 561 patients with ulcerative colitis were diagnosed with dysplasia, with 28 patients progressing to cervical cancer; in the case of Crohn’s disease, 407 patients were diagnosed with dysplasia, and 26 patients ended up developing cervical cancer.
Both ulcerative colitis and Crohn’s disease patients had a higher risk, compared to the control group, for low-grade and high-grade squamous intraepithelial lesions (SILs); an increase of cervical cancer was observed in Crohn’s disease patients only.
Finally, the authors found an increased risk for a positive diagnostic of cervical neoplasia in a period of 1 to 9 years before women were diagnosed with ulcerative colitis, when compared to the control group (women without both ulcerative colitis and Crohn’s disease).
The findings of the study show a two-way association between both forms of IBD, mainly Crohn’s disease, in developing uterine cervix neoplastic lesions.
The researchers commented, “Women with a diagnosis of CD had increased risk of cervical dysplasia and cancer despite similar screening intensity as in the general population. Patients with UC only had increased risk of dysplasia along with a slightly increased screening frequency compared to controls. Patients with IBD should be encouraged to follow the screening program for cervical neoplasia and clinicians should be aware of the slightly increased risk of HPV-related cervical lesions in IBD patients.”