The risk that inflammatory bowel disease (IBD) patients will develop non-alcoholic fatty liver disease (NAFLD) increases as IBD worsens, according to Italian researchers.
Their study “Non-alcoholic fatty liver disease phenotypes in patients with inflammatory bowel disease,” appeared in the journal Cell Death & Disease.
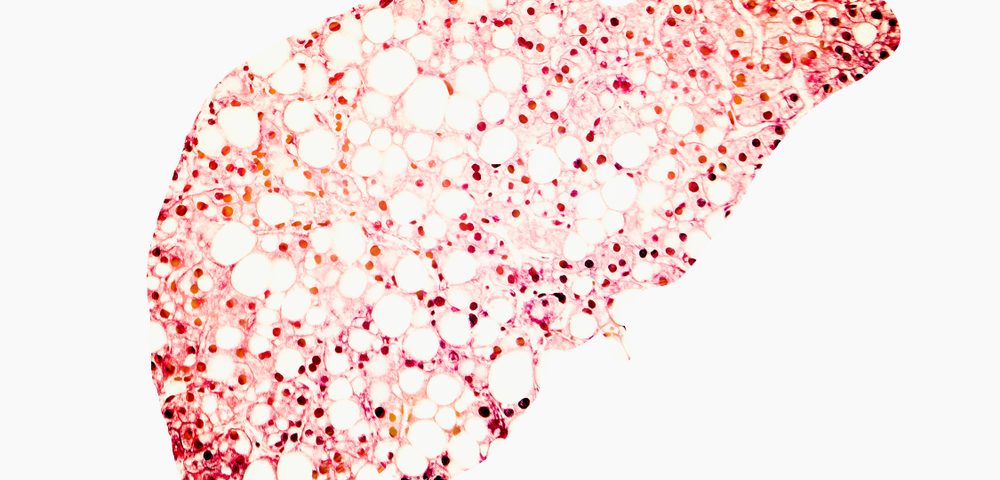
NAFLD is associated with higher risk of cirrhosis and hepatocellular carcinoma. Although the condition is more often associated with metabolism dysfunction and metabolic syndrome (MetS) — a cluster of factors that raises the risk for heart disease and other health problems, NAFLD can also be present with IBD. However, scientists generally don’t know the clinical characteristics of these patients, or how NAFLD affects IBD.
In their retrospective study, researchers at the University of Modena’s Department of Internal Medicine assessed NAFLD’s clinical and metabolic parameters in two groups — IBD patients and those without IBD — to identify specific signs for NAFLD in an IBD population.
Of the 223 patients participating, 78 had both NAFLD and IBD; the remaining 145 patients were diagnosed with NAFLD only. Of the 78 with both conditions, 42 had Crohn’s disease and 36 ulcerative colitis.
Among IBD patients, 55.1 percent had extensive disease, while 33.3 percent had active disease lasting at least three months. In addition, 25 of the 34 patients with more than one disease flare per year had been treated with corticosteroids — either budesonide (Pulmicort) or beclomethasone (Qvar).
Patients with NAFLD and IBD were generally younger than those with only NAFLD, the data showed. These patients were less prone to show liver damage but carried higher levels of inflammatory markers, including C-reactive protein, and more immune cells — specifically white blood cells and platelets.
This phenomenon is likely due to the number of patients with active IBD. The pool of NAFLD and IBD patients also had lower mean body weight, smaller waist circumference and lower body mass index. Among NAFLD patients without IBD, 56.6 percent had metabolic syndrome, versus 23.1 percent of those with IBD. Yet 32.1 percent of those with IBD showed severe steatosis (fatty liver) by ultrasound, versus 16.6 percent of NAFLD patients without IBD.
“These features indicate that NAFLD in IBD patients is notably different from what is observed in patients without IBD,” researchers wrote. Independent risk factors for severe steatosis by ultrasound in IBD patients included more than one IBD relapse per year during disease history, surgery for IBD and more extensive intestinal involvement.
Anti-TNF alpha therapy was the only parameter found to protect against damages to the liver, researchers concluded.
“IBD patients seem to develop different NAFLD phenotypes according to intestinal disease clinical course. More severe IBD seem to predict the presence of more severe steatosis. Therapy with antiTNFα antibodies could prevent alteration of liver enzymes in such population,” they wrote. “However, future prospective studies are needed to evaluate whether such specific NAFLD phenotypes could have different prognostic course in this subgroup of patients.”