Exclusive enteral nutrition (EEN) is just as effective as corticosteroids in inducing remission in Crohn’s disease patients — including children — and with fewer adverse effects. According to a review analysis, the results support previous evidence showing that EEN is safe for use as first-line therapy for children and adolescents with the disease.
The study, “Systematic review with meta-analysis: enteral nutrition therapy for the induction of remission in paediatric Crohn’s disease,” appeared in the journal Alimentary Pharmacology & Therapeutics.
U.S. doctors commonly use corticosteroids to reverse Crohn’s disease, yet they “pose particular risks in a pediatric population” including bone thinning, weight gain and lose of muscle mass, the study’s authors wrote.
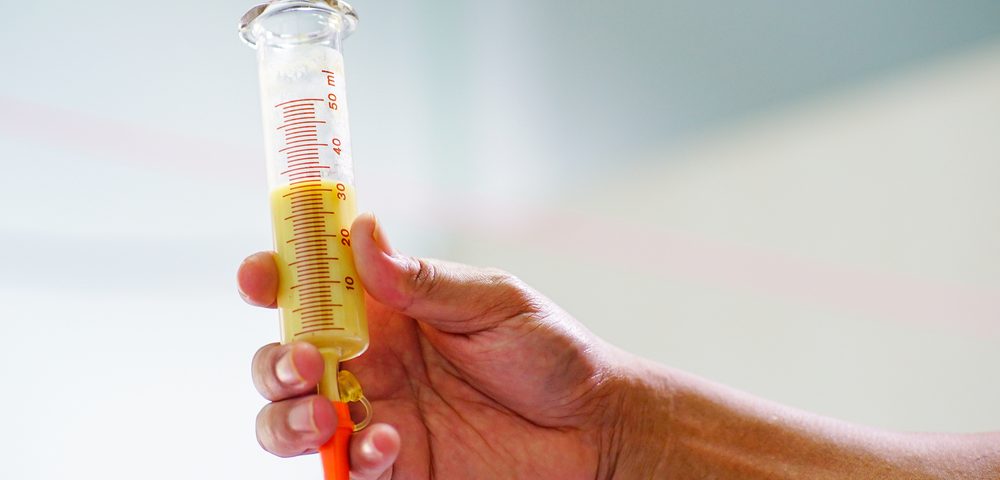
One alternative is EEN, a dietary intervention in which patients receive a liquid diet of formula, either orally or via nasogastric tube. Despite its effectiveness, the use of EEN to treat Crohn’s disease in North America is limited.
Authors performed a systematic review and analysis to compare the efficacy of corticosteroids versus EEN among children, with the primary goal of assessing the level of remission achieved by each therapy.
They searched studies published in eight online databases. Out of 2,795 identified sources, they selected eight studies for analysis.
Results showed no differences in efficacy between EEN and corticosteroids in inducing remission of Crohn’s in children. Moreover, in their analysis, authors observed that children treated with EEN showed superior intestinal mucosal healing.
“EEN may have the added benefit of minimizing growth failure, avoiding undesirable and difficult-to -everse changes to body habitus, and can potentially result in a deeper and longer duration of remission,” authors concluded, urging “greater advocacy” for EEN among U.S. physicians.
“The most common question in a newly diagnosed patient is, ‘what should I eat?'” Dr. Arun Swaminath, the study’s lead author, said in a news release. “This would be an ideal time to discuss this treatment option, especially in pediatric populations, but it does require a motivated patient and a supportive team — typically composed of a dietician, nurse, and physician, and often, family/peer supporters — to make it all happen.”