Researchers identified a gene, known as multidrug resistance-1 (MDR1), that may underlie the most severe and incurable forms of inflammatory bowel diseases (IBD). The findings may lead to the development of new therapies for IBD patients.
The study “MDR1 deficiency impairs mitochondrial homeostasis and promotes intestinal inflammation” was published in the journal Mucosal Immunology.
The MDR1 gene carries vital functions in the gut by preventing the cells’ uptake of damaging substances or by promoting the substances’ rapid elimination.
Researchers at the University of Edinburgh looked at the expression of MDR1 in IBD patients and compared it to biopsies of the colon from patients with inflamed IBD, to those who showed no signs of inflammation. They found that MDR1 function was decreased in inflamed colons of IBD patients.
To understand the significance of a lower expression on MDR1 in the colon, researchers used mice that lack MDR1 altogether. These mice, they learned, had defective mitochondria.
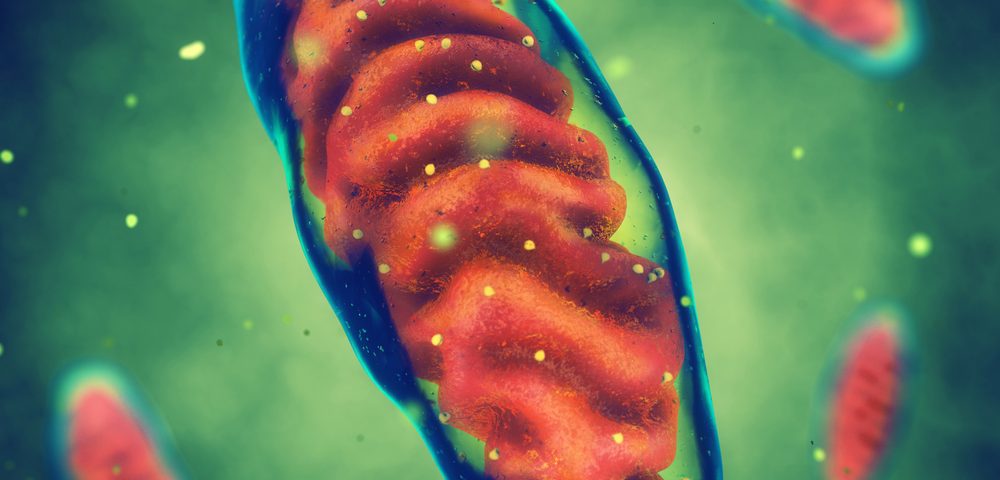
Mitochondria are small organelles that exist inside cells and perform vital functions; one of the most important being the production of energy cells needed to function properly and protect against damaging molecules, known as reactive oxygen species (ROS).
Defective mitochondria, upon loss of MDR1 function, led to the development of colitis, the inflammatory status in the colon that defines IBD. Researchers performed more in-depth studies and found that “many (∼5%) of IBD susceptibility genes with direct roles in regulating mitochondria homeostasis,” they wrote in their abstract.
Moreover, the team showed that a mitochondria-targeted drug, Mitoquinone, known for its protective role, reduced colitis and promoted bowel recovery in the mice lacking MDR1.
“IBD has a serious impact on quality of life, with 6,000 new cases diagnosed per year in the U.K. We have shown that MDR1 and mitochondrial function are important jigsaw pieces in the complex causes of IBD,” Gwo-Tzer Ho, MD, honorary consultant gastroenterologist at the MRC Centre for Inflammation Research, University of Edinburg and lead author of the study, said in a press release.
“Our studies highlight the importance of shielding the mitochondria from damage. This will open new approaches to drug targets that focus on the mitochondria to better design treatments for patients,” he concluded.