Specific biologic treatments don’t only relieve symptoms but can also maintain intestinal health in patients with inflammatory bowel disease (IBD), according to a review that analyzed medicines approved by the U.S. Food and Drug Administration (FDA) to treat IBD.
The study “Systematic review with meta-analysis: comparative efficacy of biologics for induction and maintenance of mucosal healing in Crohn’s disease and ulcerative colitis controlled trials,” appeared in the journal Alimentary Pharmacology & Therapeutics.
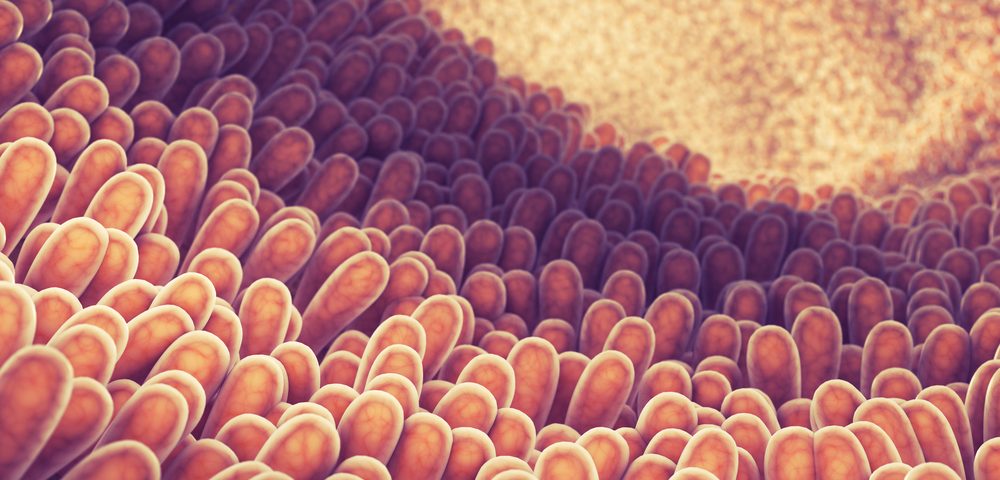
Doctors have used therapeutics mostly as a means to relieve patients of IBD-related symptoms. Recently, however, this strategy is shifting and IBD treatments increasingly target intestinal mucosal healing. This is because in many cases, the mucosa — or inner layer of the gastrointestinal tract — often remains ulcerated, with patients ultimately requiring surgery.
While several drugs are approved IBD therapeutics, researchers weren’t sure which were best at healing the intestinal mucosa. Now, a team of researchers has performed a systematic review and analysis of randomized controlled trials investigating mucosal healing with different treatments.
Specifically, the study aimed to “examine the efficacy of each therapeutic class in inducing and maintaining mucosal healing in moderate-to-severe Crohn’s disease and ulcerative colitis (UC), and to perform network meta-analysis utilizing direct and indirect evidence from clinical trials to derive comparative efficacy of various therapies in achieving mucosal healing.”
The analysis included only FDA-approved therapies for treatment of Crohn’s or UC: Imuran (azathioprine), Trexall (methotrexate), Purinethol (mercaptopurine), Remicade (infliximab), Humira (adalimumab), Cimzia (certolizumab), Simponi (golimumab), Tysabri (natalizumab) and ENTYVIO (vedolizumab).
In total, 12 randomized controlled trials were included in the meta-analysis. Researchers found that, in general, Remicade and Humira — both targeting the TNF-alpha — were much more effective at maintaining mucosal healing in Crohn’s when compared to placebo controls (28% versus 1%, respectively.)
For ulcerative colitis, medicines targeting both TNFs and integrins (proteins involved in cellular adhesion and stability) were more effective than placebo controls in inducing (45% versus 30%) and maintaining (33% versus 18%) mucosal healing.
Importantly, researchers found that in UC, Humira was inferior to Remicade for the induction of mucosal healing, while both medicines were similar in CD.
“We demonstrate that both anti-TNF and anti-integrin biological agents are effective for inducing and maintaining mucosal healing in UC, and anti-TNF therapies in CD,” authors concluded. “However, between-drug differences in efficacy exist within each therapeutic class, particularly for induction of mucosal healing in UC, mucosal healing infliximab or combination therapy being the preferred strategy.”