Editor’s note: In the final installment of her four-part series, Mary Horsley writes about Crohn’s disease medications.
After noting symptoms, getting a diagnosis, and, coping with that Crohn’s disease diagnosis, you may begin researching treatments and medications. It gets scary and confusing for all of us Crohnie’s in the beginning; don’t worry.
With Crohn’s medications, your doctors may suggest a different treatment plan than I tried. I cannot, and would not, offer medical advice, I can only share what I know from my personal experiences.
But you have to remember, Crohn’s disease has no cure.
Some doctors use a pyramid-style treatment plan, starting with medications that have the least number of side effects, the least harmful at the bottom. Other doctors use the same pyramid, but upside down, with the more aggressive medications first, but these also are more harmful.
Depending on how your disease and treatment progress, the location of your Crohn’s, and the circumstances related and decisions made by you and your doctor, there are a plethora of medications to try.
Here are some Crohn’s medications, and some I have tried:
5-amniosalicylates, or 5-ASAs
Before diagnosis, doctors already may have started you on medications for your Crohn’s disease, in hopes they can prevent more inflammation before it begins.
Sulfasalazine and mesalamine are anti-inflammatory medications under the 5-ASA title. These medications are used to help manage mild symptoms related to Crohn’s, like diarrhea, stomach pain, and other issues. These medications help by releasing medicine in specific areas of the colon and intestines.
When those didn’t work for me, I found out I was allergic to sulfa drugs and I suffered a number of other side effects, like nausea and migraines. After seeing a new GI doctor, I began a new treatment plan.
Corticosteroid and Steroids
 Budesonide, a capsule corticosteroid, helps to control the symptoms caused by Crohn’s by targeting a very specific area of the right side intestine. The downfall, a year after, it is if you never took the medication at all. This means you will have future flaring, guaranteed. I was put on budesonide for three months without a change in my symptoms. I began to suffer vomiting and more nausea, so I was given prednisone until we found a treatment that worked for me.
Budesonide, a capsule corticosteroid, helps to control the symptoms caused by Crohn’s by targeting a very specific area of the right side intestine. The downfall, a year after, it is if you never took the medication at all. This means you will have future flaring, guaranteed. I was put on budesonide for three months without a change in my symptoms. I began to suffer vomiting and more nausea, so I was given prednisone until we found a treatment that worked for me.
Prednisone also is a steroid widely used with Crohn’s patients to help induce remission and stop inflammation. These steroids cannot be used long term due to their complications and adverse side effects, but they usually act fast to bring some relief to those suffering symptoms. Prednisone is normally paired with another medication.
My doctor suggested a capsule endoscopy before and after the budesonide treatment to compare inflammation imaging. Once I had finished my trial of the medication and my results in, my Crohn’s had gotten worse. Next step up the pyramid, I go.
Immunosuppressants or Immunomodulators
These medications start to get more serious. They begin to weaken the immune system further, trying to stop its overactive response that is creating the Crohn’s inflammation.
Medications like Azathioprine and Methotrexate prevent the immune system from working fully, trying to prevent bad activity while suppressing the good, too. This means you can become sick easier or suffer more side effects, but you have a greater chance of finding relief.
Azathioprine is offered in pill form; while methotrexate is an injection. This is often where Crohn’s patients learn how to inject themselves with medicines at home.
I still take azathioprine, but I have never tried Methotrexate, as it is not good for women who are trying to conceive. It is important to watch kidney and liver panel tests with these medications, as they can be harmed.
Anti-Tumor Necrosis Factor Therapy
 Humira and Remicade are two Anti-TNF medicines I have tried, although more exist. These medications are considered to be biologic drugs and used only after other medications have failed, due to the risk of harmful side effects. Anti-Tumor Necrosis Factor drugs block TNFα, the inflammatory protein that is seen in a lot of us Crohnie’s.
Humira and Remicade are two Anti-TNF medicines I have tried, although more exist. These medications are considered to be biologic drugs and used only after other medications have failed, due to the risk of harmful side effects. Anti-Tumor Necrosis Factor drugs block TNFα, the inflammatory protein that is seen in a lot of us Crohnie’s.
Humira is offered via injection, either pen or a syringe, and it is self-administered by the patient bi-weekly, either in the stomach or in the thigh. I have been told the stomach hurts less, but I never tried my thighs to compare. Starting with four shots initially, then two, then one, patients can find relief as early as the completion of the doses.
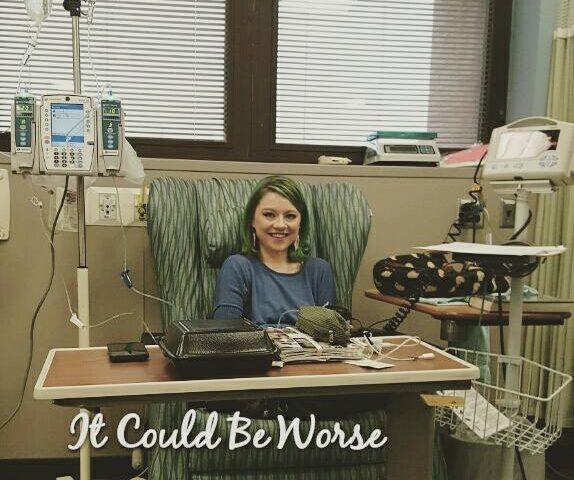
 Remicade is an IV infusion that usually takes place in your hospital chemotherapy ward. Remicade, like Humira, requires a loading dose, with infusions at week 0, 2, 4, and the treatment continuing every eight weeks.
Remicade is an IV infusion that usually takes place in your hospital chemotherapy ward. Remicade, like Humira, requires a loading dose, with infusions at week 0, 2, 4, and the treatment continuing every eight weeks.
The infusion itself takes a few hours, beginning with some hydrocortisone before the Remicade is mixed. The Remicade is made at the infusion based on weight and has been known to help patients significantly.
Both have their positives and both have side effects, but you should discuss the options with your doctor. Both can cause migraines or nausea, so keep your other medications (like Promethazine) nearby.
Remember, my Crohn’s disease is individual for me, and what works for me does not necessarily work for you. I am still searching for remission and I have my fourth Remicade infusion Friday.
For me, It Could Be Worse.
Note: IBD News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. The opinions expressed in this column are not those of IBD News Today, or its parent company, BioNews Services, and are intended to spark discussion about issues pertaining to inflammatory bowel disease.