Electrically stimulating the vagus nerve could help control inflammation in certain diseases — including inflammatory bowel disease (IBD) — according to a new study, and researchers have developed a device that allows the nerve to be stimulated electrically without triggering unwanted side effects.
“Kilohertz Frequency Nerve Block Enhances Anti-Inflammatory Effects Of Vagus Nerve Stimulation” was published in the journal Scientific Reports.
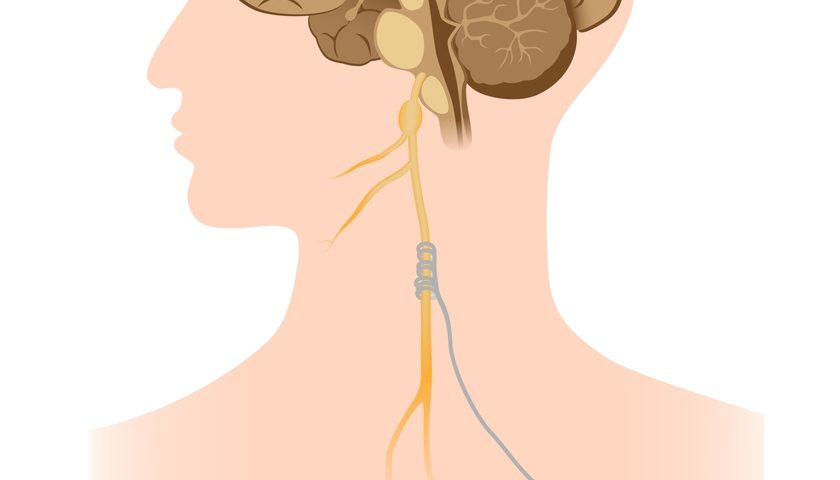
The vagus nerve passes through the neck and thorax to the abdomen, and it works by passing electrical signals between the brain and the visceral organs, such as the stomach, lungs, and heart. It’s responsible for conveying information on the state and function of those organs, controlling their activity, and “telling” the brain when something is wrong. It also regulates the immune system.
Inflammatory diseases such as IBD are characterized by excessive activation of inflammatory pathways, which can damage healthy tissues. The vagus nerve controls inflammation, so stimulating it could potentially temper swelling and help manage IBD symptoms.
Treatments based on activating the vagus nerve have been tested before in patients. But the nerve also includes a pathway that promotes inflammation, so its activation can be counterproductive.
“The original studies in animals on the anti-inflammatory benefits of vagus nerve stimulation resorted to nerve transections to achieve directional stimulation as well as boost effectiveness of nerve stimulation,” Yogi Patel, the study’s lead author, said in a news release. “But cutting the vagus is not clinically viable — due to the multitude of vital bodily functions it monitors and regulates. Our approach provides the same therapeutic benefit, but is also immediately reversible, controllable, and clinically feasible.”
Stimulating the nerve path from the brain toward other organs helps relieve chronic inflammation, while activating the path from the organs to the brain results in the production of inflammatory molecules.
Researchers at the Georgia Institute of Technology developed a device, similar to a pacemaker, that stimulates the vagus nerve. They minimized the number of unwanted side effects by inhibiting the nerve that would contribute to inflammation. The team said the inhibiting signal could increase the clinical efficacy and therapeutic benefit of this kind of treatment.
“We use an electrode with a kilohertz frequency that blocks unwanted nerve conduction in addition to the electrode that stimulates nerve activity,” said Robert Butera, senior researcher for the study. “We’ve arranged the two near each other, so the blocking electrode forces the stimulation from the stimulating electrode to only go in one direction.”
The device was tested in rats, and the results were promising, including a marked decrease in inflammation. No other measures had to be taken to decrease inflammation, such as cutting part of the nerve.
According to the researchers, stimulation using the device can be turned on or off, and it can be tuned according to the specific needs of each patient.