Recently, researchers from the University Medical Center Utrecht in the Netherlands released results from a comparative study that looked at the capacity of tests to detect colorectal dysplasia in inflammatory bowel disease (IBD). Their research suggests that Chromoendoscopy for surveillance in patients with inflammatory bowel disease (IBD) does not increase detection of dysplasia compared with conventional white light endoscopy with random biopsy sampling. The study entitled, “Chromoendoscopy for Surveillance in Inflammatory Bowel Disease Does Not Increase Neoplasia Detection Compared with Conventional Colonoscopy With Random Biopsies: Results From a Large Retrospective Study,” was published in the latest edition of the American Journal of Gastroenterology.
Background Terminology:
- Colorectal dysplasia: condition in which the cells within the colon have become abnormal. These abnormal cells are considered to be pre-cancerous.
- White light endoscopy (WLE): endoscopy (an instrument used to examine the interior of the digestive tract) procedure using light to detect abnormal cells.
- Chromoendoscopy: endoscopy using dyes to detect abnormal cells.
Inflammatory bowel disease
IBD is a debilitating disease caused by chronic inflammation throughout all or part of a patient’s digestive tract. It includes:
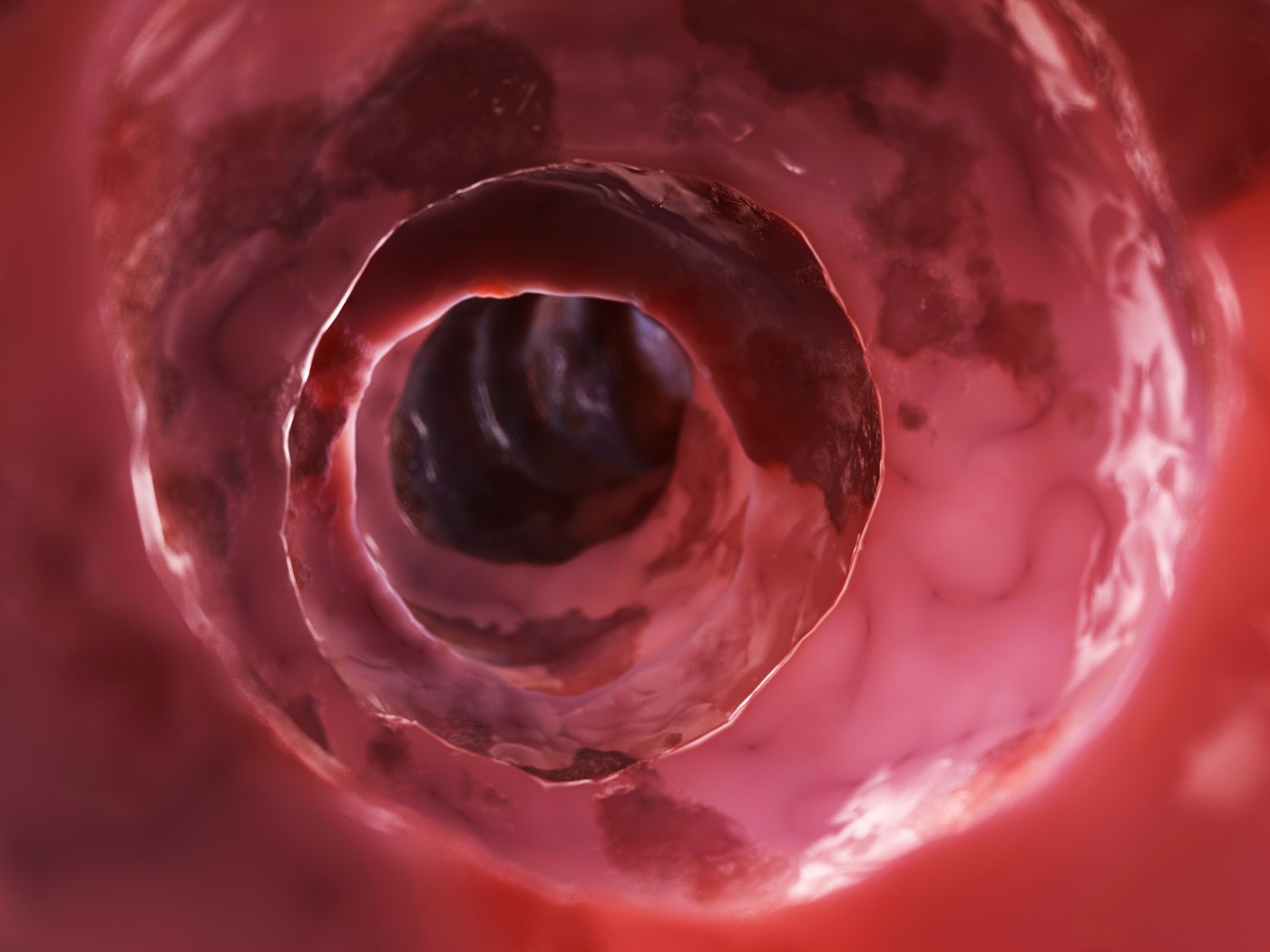
- Ulcerative colitis (UC): causes long-lasting inflammation and sores (ulcers) in the innermost lining of the large intestine (colon) and rectum.
- Crohn’s disease (CD): causes inflammation of the lining of the digestive tract. In Crohn’s disease, inflammation often spreads deep into affected tissues. The inflammation can involve the large intestine, small intestine or both.
Patients with IBD are at increased risk for developing colorectal cancer. It is therefore important for both patients and their physicians that surveillance methods to detect pre-cancerous dysplasias during endoscopic procedures be precise and successful.
This Study
To assess the rate of dysplasia detection by chromoendoscopy in comparison to those detected by WLE, the researchers reviewed the charts of 937 patients (2242 procedures) with IBD (35% Crohn’s disease; 65% ulcerative colitis) who underwent endoscopic surveillance between January 2000 and November 2013 by the following methods:
- WLE was performed in 772 patients (1,802 procedures).
- Chromoendoscopy was performed in 401 patients (440 procedures).
The medical chart reviews established whether patients had a valid indication for colorectal cancer screening, as well as obtaining the patients’ demographics, date of IBD diagnosis, type of IBD, disease extent before the start of surveillance, and family history of colon cancer.
The primary study findings showed that implementation of chromoendoscopy for IBD surveillance did not increase dysplasia detection compared with WLE in this population of patients. Other findings included:
- Dysplasia was detected in 11% of chromoendoscopies compared with 10% of WLEs.
- Targeted biopsies identified neoplasia in 11% of chromoendoscopies compared with 9% of WLEs.
- Risk factors for IBD-related colorectal cancer were comparable between chromoendoscopy and WLE groups.
- Patients with a first-degree relative diagnosed with colorectal cancer was higher in the chromoendoscopy group.
- A greater number of patients with CD with extensive colitis was found in the chromoendoscopy group.
When discussing their findings the authors wrote, “In conclusion, we did not find an increase in neoplasia detection after the implementation of chromoendoscopy as compared with the conventional white light endoscopy plus random biopsies protocol. Although more studies are needed to confirm this and our results could be biased because of the retrospective nature of our study, these results cast doubt on the standard use of chromoendoscopy as the preferred surveillance tool in IBD.”