 Inflammatory Bowel Disease (IBD) is one of the main focuses at Penn State Hershey Children’s Hospital, part of a national network that works to improve treatment for pediatric IBD patients. The program includes a multidisciplinary team composed of doctors, nutrition specialists, as well as psychologists and social professionals to help children with IBD cope with the challenges of living with the disease.
Inflammatory Bowel Disease (IBD) is one of the main focuses at Penn State Hershey Children’s Hospital, part of a national network that works to improve treatment for pediatric IBD patients. The program includes a multidisciplinary team composed of doctors, nutrition specialists, as well as psychologists and social professionals to help children with IBD cope with the challenges of living with the disease.
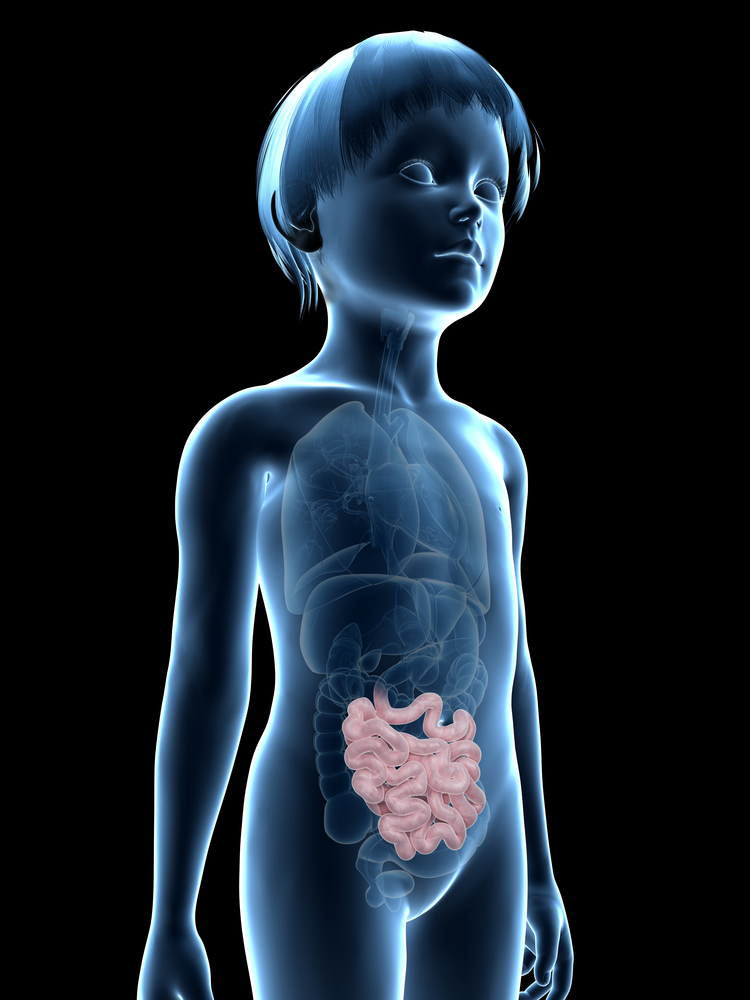
Doctors note that when a child presents frequent stomach aches (occurring for more than a few weeks) and are accompanied by additional symptoms and bloody stools they are probably caused by IBD. The disease includes a group of syndromes characterized by chronic inflammation, particularly of the colon and small intestine. The two main types of IBD are Crohn’s disease (CD) and Ulcerative Colitis (UC).
In children, Crohn’s disease commonly leads to impaired child growth and weight gain. The diagnosis usually includes children experiencing painful stomach aches with occurrences of diarrhea or bloody stools.
Dr. Marc Schaefer, a pediatric gastroenterologist specializing in IBD at Penn State Hershey Children’s Hospital noted in a press release, “Growth charts are one of the most important things we look at with children because sometimes a slower growth rate is the only sign of IBD, especially with Crohn’s disease,” aided by blood tests and endoscopy to accurately diagnose children with Crohn’s disease.
While the etiology of IBD is unknown, both environmental and genetic factors are known to play a role in disease development, increasing chances of children carrying the disease if IBD runs in the family. However, disease occurrence as well as severity is variable within families, with the occurrence of long asymptomatic periods followed by sporadic or recurrent disease flare-ups.
Doctors highlight that in fact IBD is a chronic disease that needs monitoring throughout life, but several lines of treatments are currently available. These include pills, liquid medications, injections or infusions; additionally, while certain types of foods can exacerbate patients’ symptoms, no diet alone can actually cure IBD. The treatment for IBD has to be personalized for each patient, as noted by Dr. Marc Schaefer “We really individualize the treatment and tailor it to each patient. We have to factor in results of endoscopies as well as the severity and behavior of the disease. What might work for one patient may not be best for another.”
The work performed at Penn State Hershey Children’s Hospital in their IBD transition clinic is to help children learn how to manage their disease as they become adults.
Dr. Tolulope Falaiye, also a pediatric IBD specialist at Penn State Hershey added, “There are a lot of things they need to start doing for themselves and the transition clinic really highlights for the family the changes that are coming.”