 A new study entitled “Diffuse filiform polyposis of the small intestine without inflammatory bowel disease” was published in the World Journal of Surgical Oncology by Jin-Wei part of Dr. Yu-Jie Zhang’group from the Department of General Surgery, Sir Run Run Shaw Hospital, School of Medicine, Zhejiang University, Hangzhou, China, and colleagues. The findings from this study offer new insights into how medical practitioners can effectively deal Filiform polyposis in a variety of different health settings.
A new study entitled “Diffuse filiform polyposis of the small intestine without inflammatory bowel disease” was published in the World Journal of Surgical Oncology by Jin-Wei part of Dr. Yu-Jie Zhang’group from the Department of General Surgery, Sir Run Run Shaw Hospital, School of Medicine, Zhejiang University, Hangzhou, China, and colleagues. The findings from this study offer new insights into how medical practitioners can effectively deal Filiform polyposis in a variety of different health settings.
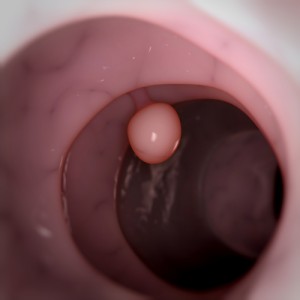
Filiform polyposis is a rare form of pseudopolyposis — finger-like projections that develop from newly formed connective tissue and blood vessels during the healing process in frequent cycle of ulceration, associated with ulcerative colitis, Crohn’s disease, or granulomatous disease, formed by non-specific mucosal and submucosal reactions to prior severe inflammation. This condition is mostly asymptomatic and is usually diagnosed on colonoscopy. Filiform polyposis normally occurs in patients with inflammatory bowel disease although it can also happen in patients with no inflammatory bowel disease.
In this study, the research team presented a case of a man with 56 years of age with no history or evidence of inflammatory bowel disease but with filiform polyposis of the small intestine. The main symptoms of the patient were melena, i.e. bloody feces that are normally associated with upper gastrointestinal bleeding, and anemia. They performed an urgent investigative laparotomy where finger-like polyps along the all small intestine were observed. In addition the researchers performed a partial excision of the small intestine to treat the bleeding in the bowel. Two days after the intervention the patient showed recurrent melena, and an abdominal angiographic embolization, a procedure to occlude the blood vessels, was performed with success ending the bleeding.
The research team performed a histological analysis of the removed tissue sample and observed the presence of chronic inflammatory cells inside the lamina propria with no hyperplastic or adenomatous epithelial alterations. The careful management of the patient with regular follow-up examinations was suggested due to the great risk of bleeding recurrence.

