A new study entitled “An in vivo model of human small intestine using pluripotent stem cells” published in the online issue of Nature Medicine reports on the development of a model of the human small intestine from pluripotent stem cells.
A new study entitled “An in vivo model of human small intestine using pluripotent stem cells” published in the online issue of Nature Medicine reports on the development of a model of the human small intestine from pluripotent stem cells.
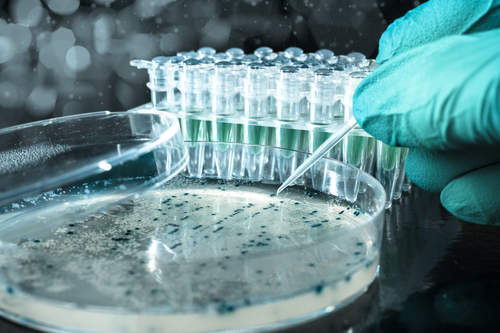
Organoids are organ-buds that are cultivated in a laboratory and used in regenerative medicine. The ability to build human organoid structures from differentiated human pluripotent stem cells (hPSCs) is the ultimate goal of many current investigations that would allow the study of human diseases, pharmacological studies, and therapeutic transplants.
In this study, the team of scientists at the Department of Pediatric General and Thoracic Surgery, Cincinnati Children’s Hospital Medical Center, Cincinnati, Ohio, USA generated human intestinal organoids from both embryonic stem cells (ESCs) or induced pluripotent stem cells (iPSCs). Specifically, the authors used skin and blood adult cells and reprogrammed them to function as iPSCs, cells that can propagate indefinitely and generate, under appropriate conditions, to any cell type in our body. In the study, iPSCs were successfully differentiated into human intestinal organoids. When the in vitro-generated organoids were engrafted into the mouse kidney, the blood supply allowed the engraft to grow into a mature human intestinal tissue with crypt-villus architecture and laminated human mesenchyme. The transplanted organoid differentiated into intestinal cell lineages — enterocytes, goblet cells, Paneth cells, tuft cells and enteroendocrine cells — which was accompanied by digestive functions evidenced by studies evaluating permeability and peptide uptake. The transplanted tissue successfully responded to mouse systemic signals, following ileocecal surgery.
Michael Helmrath, MD, MS, lead investigator and surgical director of the Intestinal Rehabilitation Program at Cincinnati Children’s commented, “These studies support the concept that patient-specific cells can be used to grow intestine. This provides a new way to study the many diseases and conditions that can cause intestinal failure, from genetic disorders appearing at birth to conditions that strike later in life, such as cancer and Crohn’s disease. These studies also advance the longer-term goal of growing tissues that can replace damaged human intestine.”