 People with inflammatory bowel disease who are taking thiopurines are at significantly increased risk of lymphoma, a recent meta-analysis study showed.
People with inflammatory bowel disease who are taking thiopurines are at significantly increased risk of lymphoma, a recent meta-analysis study showed.
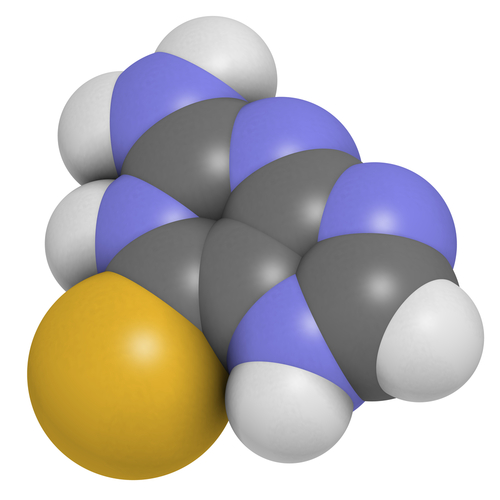
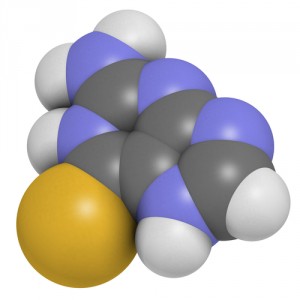
The thiopurine drugs are purine antimetabolites commonly used for the treatment of autoimmune disorders such as Crohn’s disease. There are 3 types of thiopurines that have been used for inflammatory bowel disease therapy: azathioprine, 6-mercaptopurine, and thioguanine. Although these drugs’ efficacy in the treatment of IBD has been proven, its potential toxicity has been a cause of concern for some time.
Researching this issue, a group of sixteen researchers, led by David Kotlyar of the National Cancer Institute, analyzed eighteen relevant studies regarding experimental groups that received azathiprine or 6-mercaptopurine, in order to estimate the relative risk of lymphoma in patients with IBD exposed to thiopurines, and to compare relative risk values derived from population-based studies with those from referral center-based studies. In addition, they investigated whether active use increased risk compared with past use, and whether sex, age, or duration of use influences the risk of lymphoma.
The study, entitled “Risk of Lymphoma in Patients with Inflammatory Bowel Disease Treated with Azathioprine and 6-Mercaptopurine: a Meta-Analysis,” showed that, overall, standardized incidence ratio for lymphoma was 4.49, ranging from 2.43 in 8 population studies to 9.16 in 10 referral studies. Population studies demonstrated an increased risk among current users but not among former users, with the level of risk becoming significant after 1 year of exposure. Furthermore, men were shown to have a greater risk than women, but both sexes were at increased risk for lymphoma. The higher relative risk was noted in patients younger than 30 years, with younger men having again the highest risk. However, the absolute risk was highest in patients older than 50 years.
These results led researchers to conclude that patients with IBD who are taking thiopurines have a nearly 6-fold higher incidence of lymphoma when compared to the general population. On the other hand, the increased risk does not appear to persist after discontinuation of therapy, which suggests that immunosuppression, rather than direct DNA damage, may be more of a factor in the development of excess lymphomas. In this sense, the risks of lymphoma and potential benefits of therapy should be considered for all patients with IBD.