The painful and often debilitating condition called inflammatory bowel disease (IBD) is caused by a dysregulated immune response to the host intestinal bacteria. Nan Gao, assistant professor of biology at Rutgers University-Newark (RU-N), and his colleagues are studying a specific intestinal cell called Paneth to see whether it is the cause of IBD – and if altering the behavior of the cell can eliminate the disease.
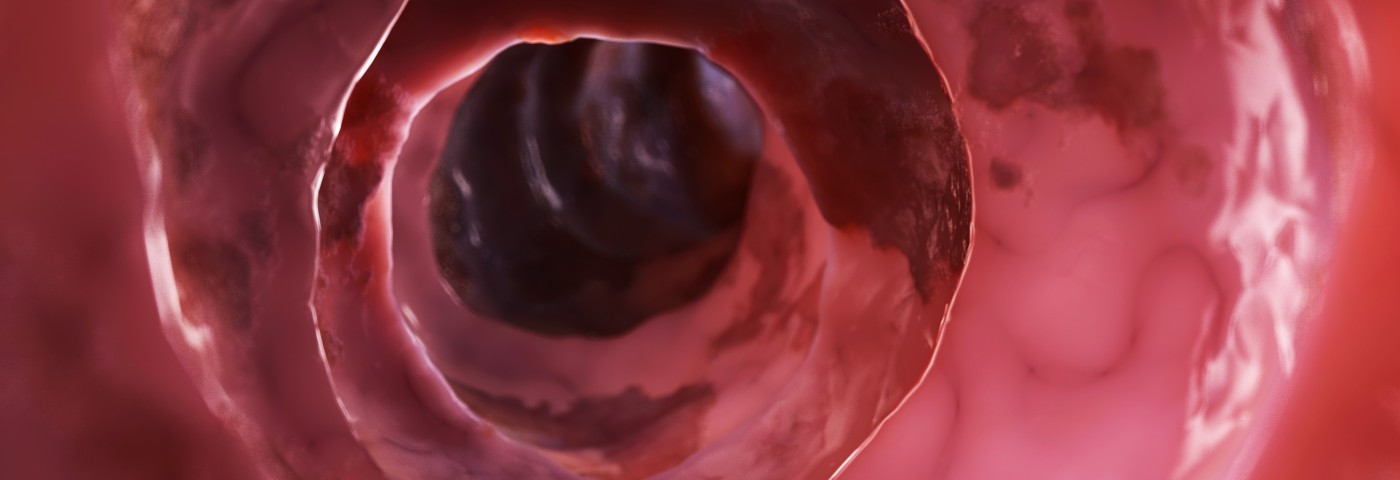
Paneth is part of the the mucosal layer that lines the intestinal wall, and has the immune function to emit anti-microbial peptides to destroy bacteria that live in the gut. The normal functioning of Paneth cells creates a defense for the intestinal wall against bacteria invasion.
When the functioning of the Paneth cell is impaired – possibly due to gene mutations – bacteria can penetrate the intestinal wall’s lining and start degrading its main structure, which triggers the immune system to fight back. The immune response of most people is beneficial; but in some – possibly because of gene mutations – the attack is too powerful and triggers inflammation. According to Gao, in IBD the patient’s own immune system destroys the intestinal tissue.
“People (…) can suffer from abdominal pain and cramping,” GAO said in a RU-N news release. “It has a great effect on people’s lives because there is no clear treatment for it. We also believe it can lead to colon cancer.”
In 2015, RU-N provided $80,000 in funding to Gao’s lab through one of six Initiative for Multidisciplinary Research Team (IMRT) grants. His research group includes faculty members from Rutgers, including Rutgers New Jersey Medical School and the university’s Graduate Programs in Molecular Biosciences.
George Yap, associate professor of medicine at the medical school and a member of its Center for Immunity and Inflammation is one of the other researchers taking part in the study of the Paneth cell and IBD. Yap is an immunology expert with a research interest in toxoplasmosis, a parasitic disease caused by Toxoplasma gondii..
“The portal of entry of the parasite is the intestine, so the Paneth cell might also be involved in resisting the parasite,” Yap said, adding that because Gao has genetically designed a model of the Paneth cell that is well suited to lab experimentation, “we can really see what is going on.”
The research collaboration between Gao and Yap might go further, including studies on improving the understanding of gastrointestinal distress that some cancer patients undergo when they receive radiation and chemotherapy treatments. Their collaboration can also provide new insights on hospital-acquired infections.
According to Gao, if the work goes well, their research could be relevant for the development of gene therapies that can help patients by altering Paneth cell’s function. “This multidisciplinary approach makes us capable of answering some really deep questions,” he said.