A new study published in the journal Gut Pathogens revealed that human microbiota-associated mice (HMA mice) — colonized with microbes from patients suffering from ulcerative colitis (UC) — did not develop spontaneous colitis, but might be more susceptible to developing disease. The study, entitled “Development of gut inflammation in mice colonized with mucosa-associated bacteria from patients with ulcerative colitis,“ is an important step towards understanding the role of gut microbiota in UC.
Zhengyu Du and colleagues from The Czech Academy of Sciences in Prague, Czech Republic have previously investigated the effect of experimentally induced gut inflammation in normal and germ-free mice, noticing that inflammation in the germ-free mice was milder. A natural next step was to investigate the effects of inflammation in mice colonized with gut bacteria from patients with UC.
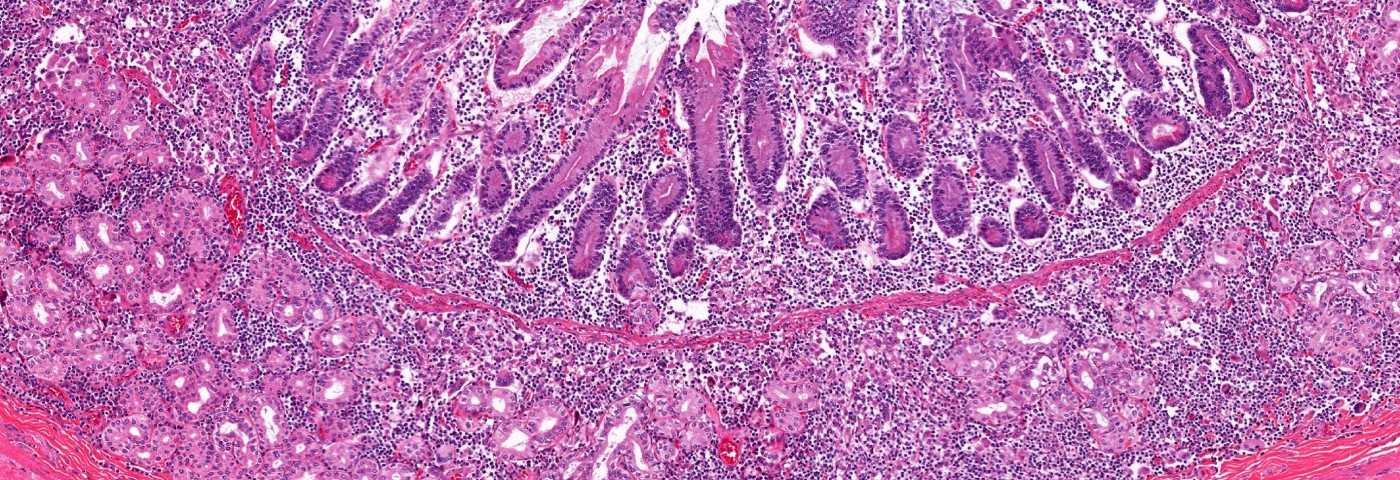
The authors of the study point out that it is the bacteria associated with the gut wall that is of interest for UC research. Bacteria usually present in the feces does not normally interact with the intestinal wall, which is protected by a thick layer of mucus. Patients with UC, however, have more bacteria in their gut wall than healthy individuals, and it is not known whether this is a result of the inflammation, or a factor contributing to the development of inflammation in the gut.
Germ-free mice were used to make sure their natural gut microbiome could not influence the result. Three mouse pairs were colonized with gut microbes from three UC patients. The mice were bred for a number of generations to study how the gut bacteria evolved over time. Following the transfer of the human microbiome to the mice, the team noticed that the number and type of bacterial species — which were similar in biopsies from all three patients — were reduced.
The team also noticed an increase in the clinical colitis score (CCS) and the activity of myeloperoxidase — an enzyme important for the antibacterial activity of neutrophil cells in the gut. These effects were not associated with any damage to the gut mucosa, and decreased in subsequent generations.
While the team could induce colon inflammation using the chemical dextran sulfate sodium (DSS), in germ-free and normal mice, they failed to do so in some of the HMA mice. Only the fourth generation of one of HMA mouse strains showed signs of colon inflammation after DSS treatment. This suggests that either the transferred bacteria have some protective properties, or that potentially harmful species were lost in the transfer. The team, therefore, analyzed the difference in bacterial species between the first and fourth generation of the HMA mice with inflammation, finding that the protective species C. symbiosum was replaced by the harmful C. difficile — associated with UC in humans.
The authors do not discuss any effects of diet — a known factor influencing gut microbiome diversity — on the composition of the bacterial species in the HMA mouse strains used in the study.
Despite the fact that the researchers could show increased sensitivity to inflammation in only one of three HMA strains, they believe that their findings are important for future studies on host-microbe interactions in UC.