An oral abstract presented on Tuesday June 9 at the International Neuromodulation Society 12th World Congress, which ran from June 6 to 11 at the Fairmont Queen Elizabeth Hotel in Montreal, Quebec, Canada, announced a new collaboration between U.S. and Chinese scientists investigating non-invasive accupoint electrical stimulation in Crohn’s disease.
The objective of a controlled clinical trial underway at the Medical University Department of Gastroenterology at the First Affiliated Hospital of Nanjing is to attempt a reduction in inflammatory response underlying the chronic gastrointestinal disorder.
The study led by gastroenterologist and principal investigator Hongjie Zhang, M.D. recruited 17 Crohn’s disease patients and 20 matched healthy controls between June 2014 and December 2014. The subjects received transdermal accupoint electrical stimulation (TAES) for an hour twice-daily, two hours after eating meals, delivered at an accupoint on the stomach meridian below the knee — the Zusanli (ST 36).
The study was initially proposed to Dr. Zhang by Jiande Chen, Ph.D. of the Division of Gastroenterology and Hepatology at Johns Hopkins Medicine in Baltimore. “We have published numerous studies showing that electrical stimulation via the acupuncture points using surface electrodes can enhance vagal activity,” he comments. “By enhancing vagal activity, we have shown in animals with intestinal inflammation that such electrical stimulation can suppress pro-inflammatory cytokines and thus reduce inflammation. Those data are being prepared for publication.”
Participants in the clinical study receive needle-less electrical stimulation through a wristwatch-sized adhesive device, powered by a watch battery. The device, which can deliver a variety of digital stimuli, was developed by Dr. Chen funded by a grant from the National Institutes of Health.
For the study’s initial three days, stimulation is administered at the hospital, after which the subjects, who have been instructed in how to use the stimulator and provided with a photo to help them identify the accupoint, are sent home, returning for evaluation at 3 days, 14 days, and 30 days. Based on data from those initial 17 patients after three days of stimulation sessions, Dr. Zhang observed an evident imbalance between sympathetic and parasympathetic branches of the autonomic nervous system.
At each evaluation, Crohn’s disease activity index (CDAI) scores are taken tracking abdominal pain, diarrhea, physical signs (i.e. average daily temperature, abdominal mass), medication use (i.e. loperamide or opiate use for diarrhea), laboratory results (such as hematocrit) and body weight.
The research team also collects blood and stool samples in order to assess levels of pro-inflammatory cytokines and gut hormones that are biomarkers of inflammation or autonomic nervous system imbalance. The effect of stimulation on autonomic nervous system balance is also non-invasively evaluated by analyzing heart rate variability.
The technique being investigated by Dr. Zhang is a form of neuromodulation — emerging therapies that employ advanced medical device technologies that act directly upon nerves by delivering electrical or pharmaceutical agents directly to a target area to enhance or suppress nervous system activity for treatment of disease. It is the alteration or modulation of nerve activity that produces the desired therapeutic effect. These technologies include implantable as well as non-implantable devices that deliver electrical, chemical or other agents to reversibly modify brain and nerve cell activity.
The program, “Neuromodulation: Medicine Evolving Through Technology,” presented at the INS Conference emphasized the field’s transformative force on the treatment of disease states — how it is approached now and how it will be in the not too distant future. Showcasing leading edge research from members of the Canadian Neuromodulation Society and from INS members around the globe, sessions on neuromodulation for pain, as well as for conditions of the neurological, cardiovascular, gastrointestinal, urological and other systems were offered.
Neuromodulation therapies are:
- Highly targeted of specific areas of the brain or spinal cord, rather than systemic throughout the body such as pharmaceutical treatments
- Highly reversible, allowing physicians to immediately cease treatment with the removal of the stimulating device
- Continuous, improving therapeutic compliance over techniques that rely on fixed intermittent dosing
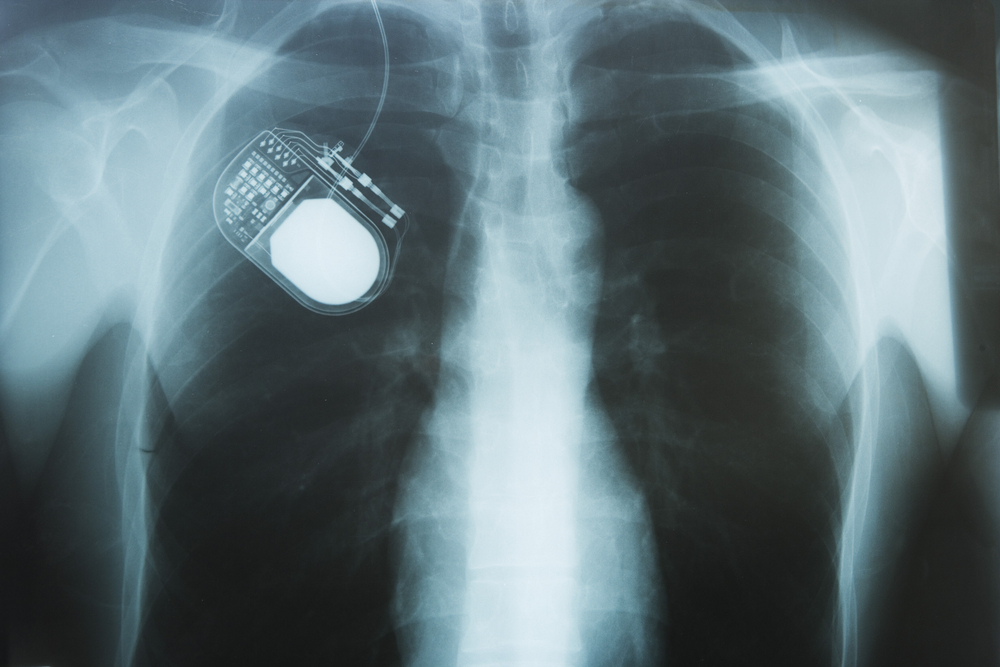
Normal neural activity is an intricate balance of electrical and chemical signals that can be disrupted by a variety of insults (genetic, chemical or physical trauma) to the nervous system, causing cognitive, motor and sensory impairments. Neuromodulation devices work similarly to the way cardiac pacemakers or defibrillators correct heartbeat abnormalities, only neuromodulation therapies help reestablish normal neural balance.
The INS notes that neuromodulation devices and treatments can be life-changing, and can be used in every area of the body and to treat nearly every disease or symptom from headaches to tremors to spinal cord damage to urinary incontinence. With such a broad therapeutic scope, and significant ongoing improvements in biotechnology, it is not surprising that neuromodulation is poised to become a major growth area for the medical industry for the next decade.
The precise nature of neuromodulation therapies enables focused delivery of modifying agents (e.g.: electrical, optical or chemical signals) to targeted areas of the nervous system in order to improve neural function. They range from non-invasive techniques such as transcranial magnetic stimulation (TMS) to techniques involving surgical implantation of devices that alter activity in discrete areas of the nervous system.
In electrical neuromodulation, precisely placed leads connect via an extension cable to a pulse generator and power source, which generates the necessary electrical stimulation. A low-voltage electrical current passes from the generator to the nerve, and can either inhibit pain signals or stimulate neural impulses where they were previously absent.
In the case of pharmacological neuromodulation, therapeutic pharmaceutical agents are delivered through implanted pumps, and drug can be administered in smaller doses than with oral administration because it does not have to be metabolized and pass through the body before reaching the target area. Conventional delivery of pain-killing drugs can be simply ineffective or become problematic for long-term use due to tolerance development, addiction, adverse side-effects or toxicity. Smaller, doses in the range of 1/300 of an oral dose administered through neuromodulation therapy can mean fewer side effects, increased patient comfort and improved quality of life.
The most common neuromodulation therapy is spinal cord stimulation to treat chronic neuropathic pain. In addition to chronic pain relief, other examples of neuromodulation therapies include:
Deep Brain Stimulation for essential tremor, Parkinson’s disease, dystonia, epilepsy and psychiatric disorders such as depression, obsessive compulsive disorder and Tourette syndrome
Sacral Nerve Stimulation for pelvic disorders and incontinence; gastric and colonic stimulation for gastrointestinal disorders such as dysmotility or obesity
Vagal Nerve Stimulation for epilepsy, obesity or depression; carotid artery stimulation for hypertension, and spinal cord stimulation for ischemic disorders such as angina and peripheral vascular disease.
Neuromodulation provides an alternative to long-term drug therapy for symptomatic relief of persistent or chronic conditions, particularly important when existing drugs are simply ineffective or become problematic for long-term use due to tolerance development, addiction, adverse side-effects or toxicity. The modern era of neuromodulation began in the early 1960s with use of deep brain stimulation (DBS) to resolve chronic and intractable pain, and evolved to include spinal cord stimulation by the end of the decade.
Neurosurgeon C. Norman Shealy has been credited with the first implantable neuromodulatory device for the relief of intractable pain in 1967. Dr. Shealy’s spinal cord stimulators, which he called “dorsal column stimulators,” were intended exclusively for pain relief, although it is noted that these early efforts were not without complications due in large part to technological and mechanical shortcomings of the new devices. However, implantable devices used for neuromodulation have steadily improved over the last four decades and recently took a major leap forward with development of rechargeable systems, smaller devices, and systems with greater but more useable complexity.
Today’s neuromodulation technologies offer the advantage of continual delivery of pharmaceutical agents, electrical signals or other forms of energy directly to the source of the condition to beneficially alter pathologic tissues behavior. Because neuromodulation therapies are so precisely targeted, they can avoid the unwanted and sometimes harmful side effects associated with more systemic or irreversible treatment of nervous system disorders. In addition, because they are easily reversible, neuromodulation therapies can provide an important degree of therapeutic control for both patients and physicians.
It has also been observed in several studies that despite the sometimes technological complexity of administering neuromodulation therapies, for some patients, early use of such therapies may actually be more cost effective for controlling certain conditions overall than conventional medical management approaches, particularly when taking into account the potential harm and associated cost of drug dependence. Examples include spinal cord stimulation for the treatment of neuropathic pain and intrathecal baclofen for the treatment severe spasticity.
As neuromodulation hardware becomes smaller and more user friendly for both doctor and patient, it seems likely that use of this avenue of therapy will grow. Indeed, the International Neuromodulation Society notes that neuromodulation devices are already the fastest growing segment of the overall medical device industry, with promising new neuromodulation therapies being developed thanks to truly multi-disciplinary, close collaboration of neuroscientists, engineers and clinicians to address such diverse disorders as migraine, obesity, obsessive compulsive disorder and depression. The 12th World Congress of the INS has brought clinicians, scientists, bioengineers and members of Industry from all over the world to Montreal, with participants from all five continents and attendance projected to surpass 1,300.
The Neurotech Business Report, which tracks the progress from medical technology to commercial products, notes that neurotechnology has now reached a level of commercial and scientific maturity that will produce enormous benefits to patients and profits to investors, and that hundreds of thousands of people have already been helped by neurostimulation products that restore hearing to deaf people, movement to individuals with paralysis, and relief to persons with chronic pain or neurological disorders. The Report projects that that the worldwide neuromodulation device industry is expected to grow from more than $6 billion in 2014 to over $10 billion in 2018, with the market for implanted spinal stimulators for treatment of chronic pain alone valued at $1.80 billion worldwide in 2014, and growing to $2.88 billion in 2018, and industry observers projecting a double-digit compound annual industry growth rate overall.
Additional co-authors of the Zhang/Chen study include Jingjing Ma, M.D. and Jiewen Su, M.D., who are contributing to the sample collection, TAES investigation, and data analysis at the First Affiliated Hospital of Nanjing Medical University. Professor Chen helped with the study design and is providing the TAES device. Dr. Zhang conceived the study and designed and supervised the experiments. The study was supported in part by the Key Medical Personnel of Jiangsu Province (no. RC2011063).
The International Neuromodulation Society (INS) is a nonprofit medical society that provides a forum and medium for clinicians, scientists and engineers to share scientific knowledge about all aspects of neuromodulation toward the goal of encouraging best medical practice. Founded in 1989 and based in San Francisco, CA, the INS presents up-to-date information about neuromodulation therapies through an interactive website at http://www.neuromodulation.com, chapter scientific meetings, the MEDLINE-indexed journal Neuromodulation: Technology at the Neural Interface, and its biennial world congress.
For more information, visit:
http://www.neuromodulation.com/medical-therapy-overview
A growing number of disorders can be treated with neuromodulation.
Patients may also read about various neuromodulation therapies.
Medical professionals, for more therapy-specific information click here.
Sources:
International Neuromodulation Society
International Neuromodulation Society 12th World Congress
Neurotech Business Report